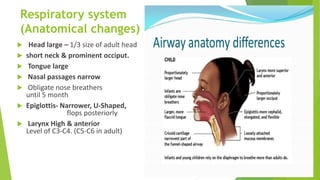
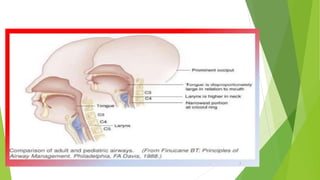
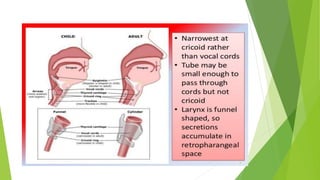
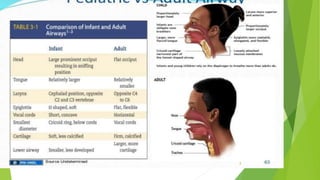
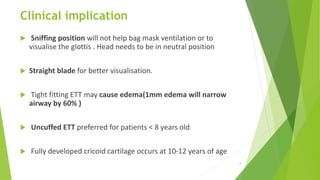
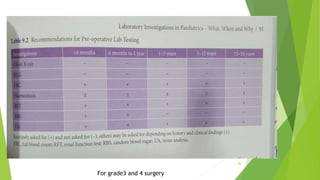
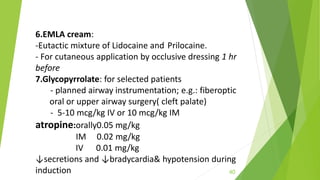
The document discusses the anatomical and physiological differences between paediatric and adult patients that are important for anaesthesiologists to consider, noting differences in the respiratory, cardiovascular, renal and other systems, as well as how these differences impact drug dosing and fluid management during anaesthesia for children. It provides guidance on preoperative assessment, induction, maintenance of anaesthesia, monitoring, fluid requirements and recovery care tailored for paediatric patients from neonates to adolescents.