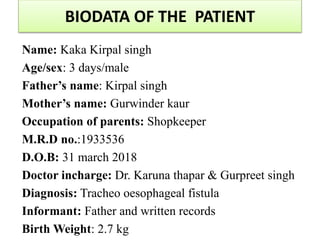
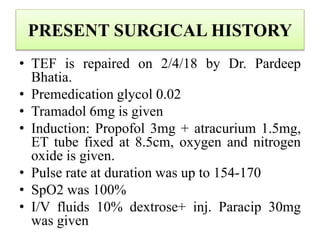
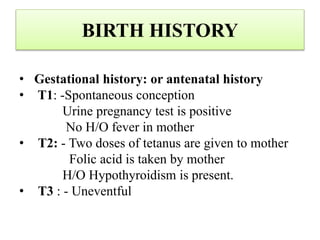
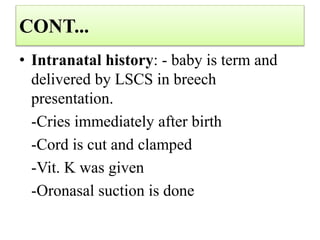
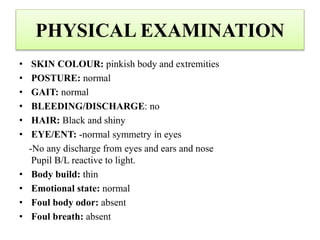
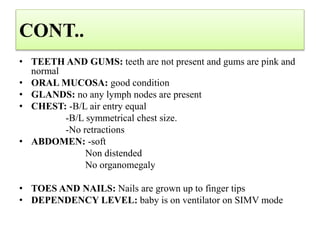
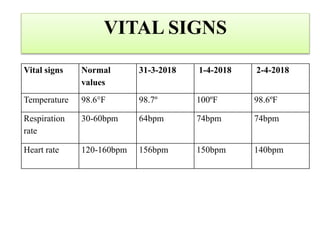
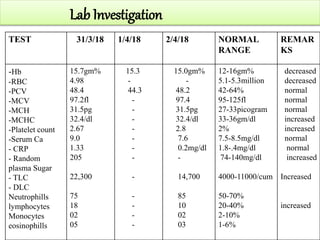
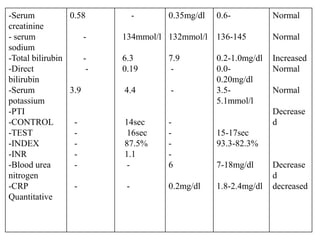
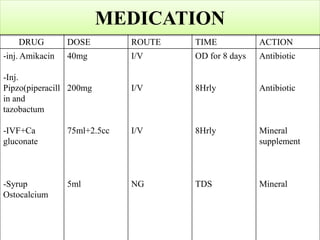
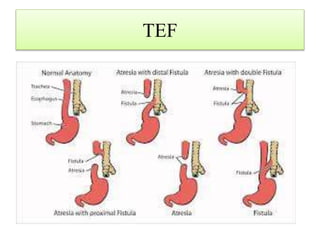
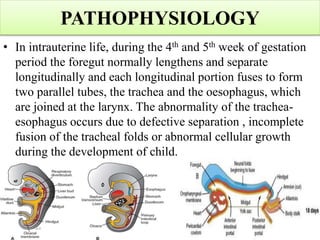
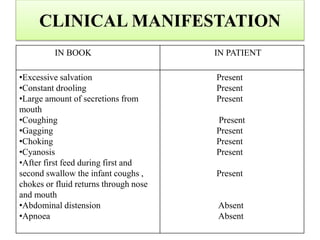
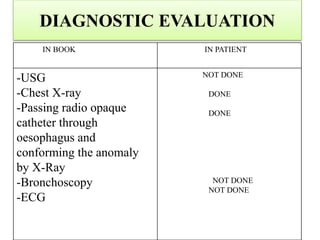
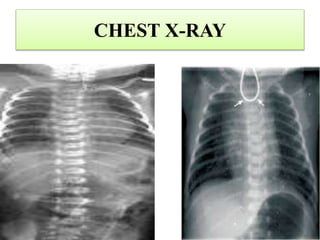
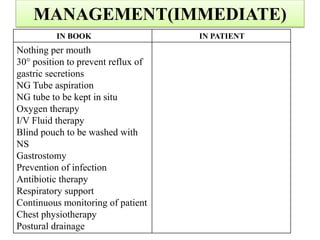
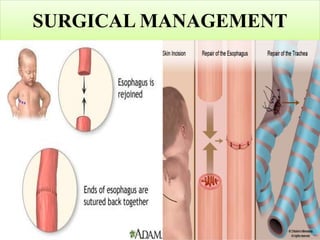
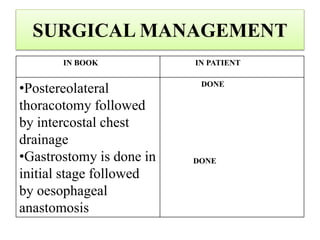
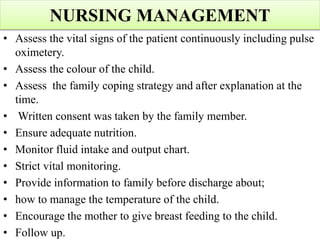
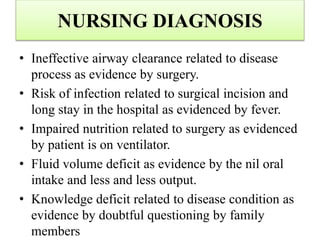
This case presentation discusses a 3 day old male infant diagnosed with tracheoesophageal fistula (TEF). The infant presented with nasal flaring, difficulty breathing, choking and cyanosis since birth. Examination and investigations confirmed TEF, which was repaired surgically. Nursing management involved strict vital monitoring, ensuring nutrition via NG tube, preventing infection, and educating the family on post-operative care.