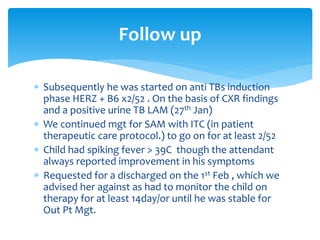
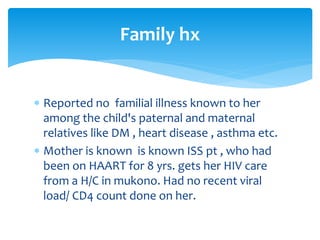
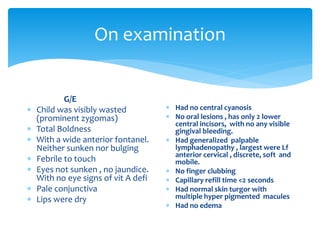
This document presents a case report of an 8-month-old male child brought to the hospital with a 3-month history of persistent cough, fever, and weight loss. On examination, the child was found to be wasted and underweight. Investigations showed anemia, lymphocytosis, and a positive urine TB-LAM test. The child was diagnosed with pulmonary TB, severe acute malnutrition, and suspected HIV infection. He was admitted and started on anti-TB treatment and therapeutic feeding for malnutrition. However, the mother discharged the child against medical advice after only a few days of treatment.




















![Investigation results
Hematologic
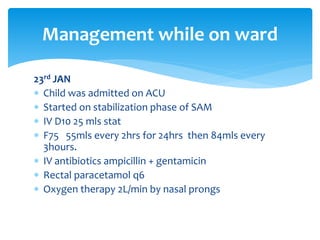
24th Jan.
BS for MPS – no MPs seen
RFTs - urea 15.5mg/dl N
- Cr 0.181mg low
Serum electrolytes
high -[k] 6.8mmol/L
-[Na] 137mmol/L
CBC 27th Jan
-WBC 15.94x10^9
-RBC normal rang
- HB 9.0g/dl
-MCV 65.4 FL
-MCH 20.5pg
-PLT 373x10^9
Lymphocytosis 48%
Neutrophils 41%
Monocytosis ……..](https://image.slidesharecdn.com/pediatrictuberculosiscasepresentation-180414130811/85/Pediatric-tuberculosis-case-presentation-24-320.jpg)