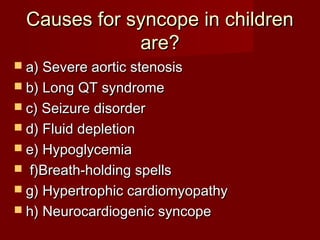
The causes listed are all potential causes for syncope in children. The most common causes are neurocardiogenic syncope, breath-holding spells, and seizures. Other important considerations include cardiac causes like long QT syndrome, hypertrophic cardiomyopathy, and aortic stenosis.