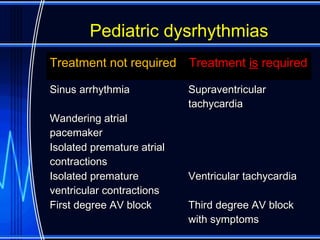
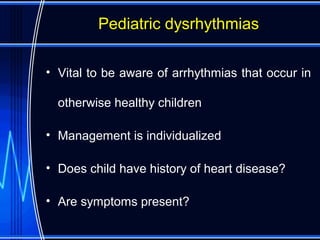
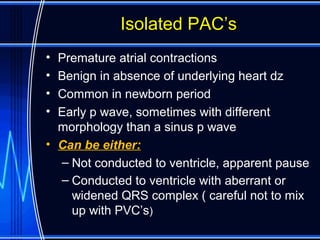
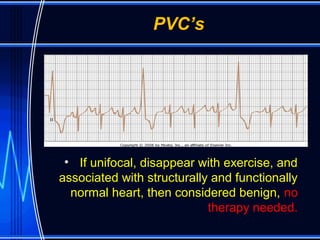
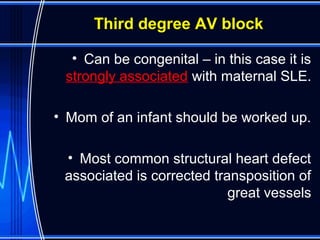
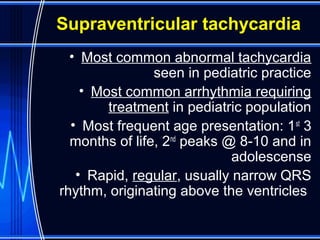
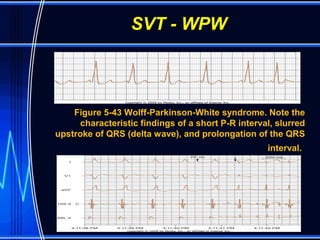
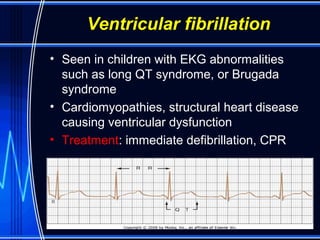
This document discusses various pediatric dysrhythmias, their typical presentations, and treatment approaches. It describes that sinus arrhythmia, wandering atrial pacemaker, and isolated premature contractions are usually normal variants that do not require treatment. Supraventricular tachycardia is the most common arrhythmia requiring treatment and can often be terminated with vagal maneuvers, adenosine, or cardioversion. First degree atrioventricular block is commonly seen in neonates but generally does not cause bradycardia. Third degree atrioventricular block may require a pacemaker, especially if associated with slower heart rates or symptoms. Ventricular arrhythmias like tachycardia or fibrillation indicate serious underlying