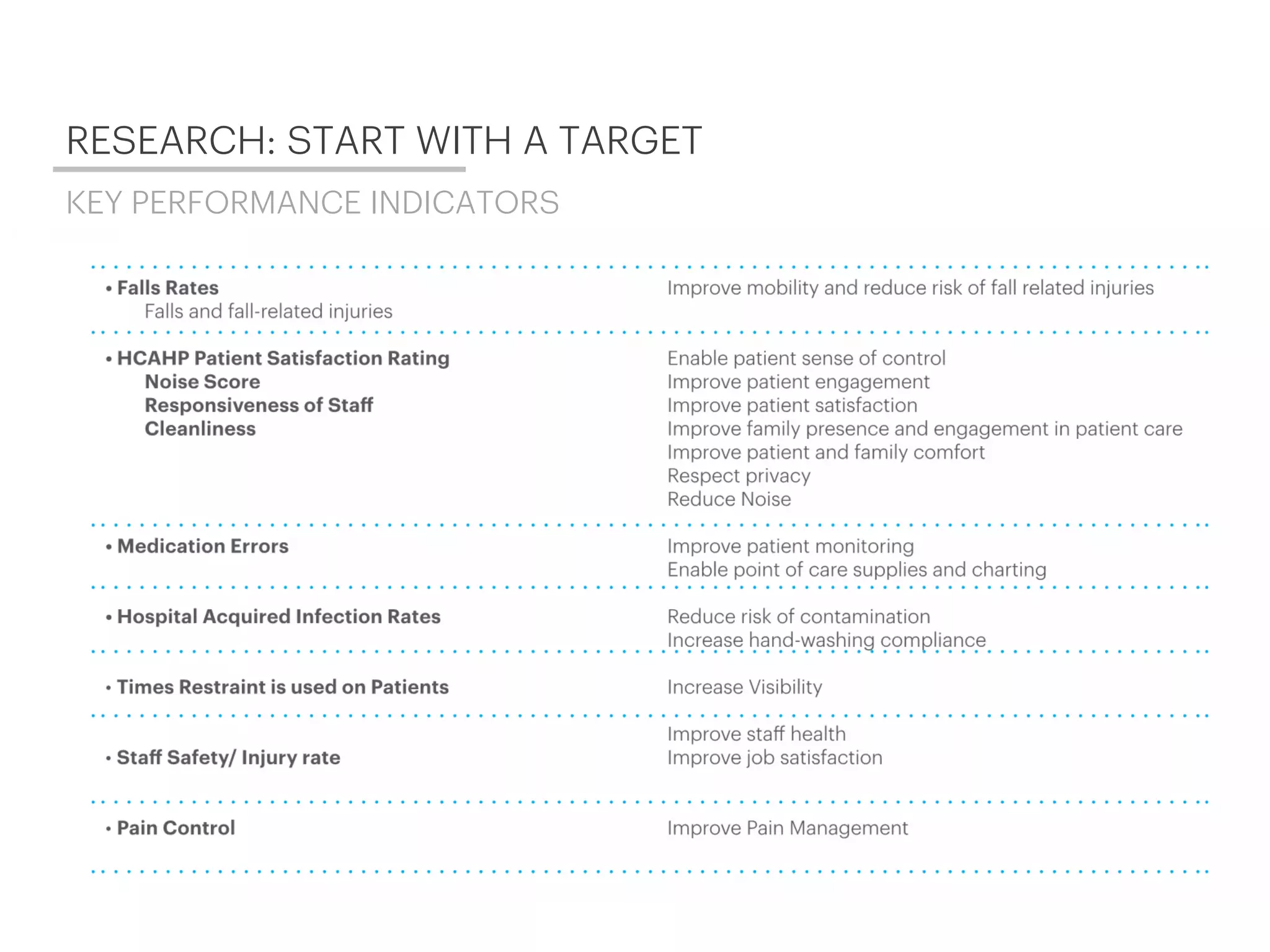
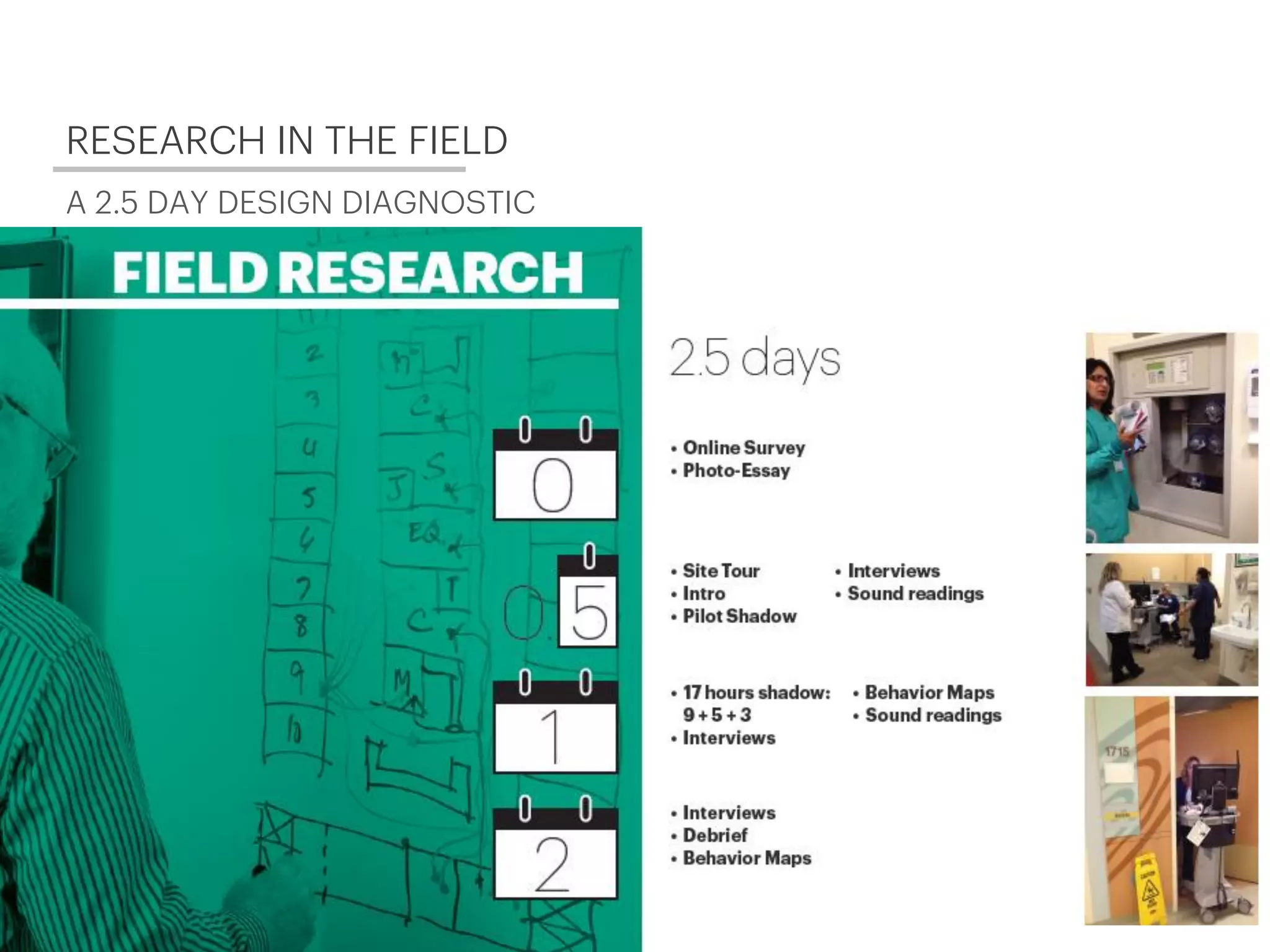
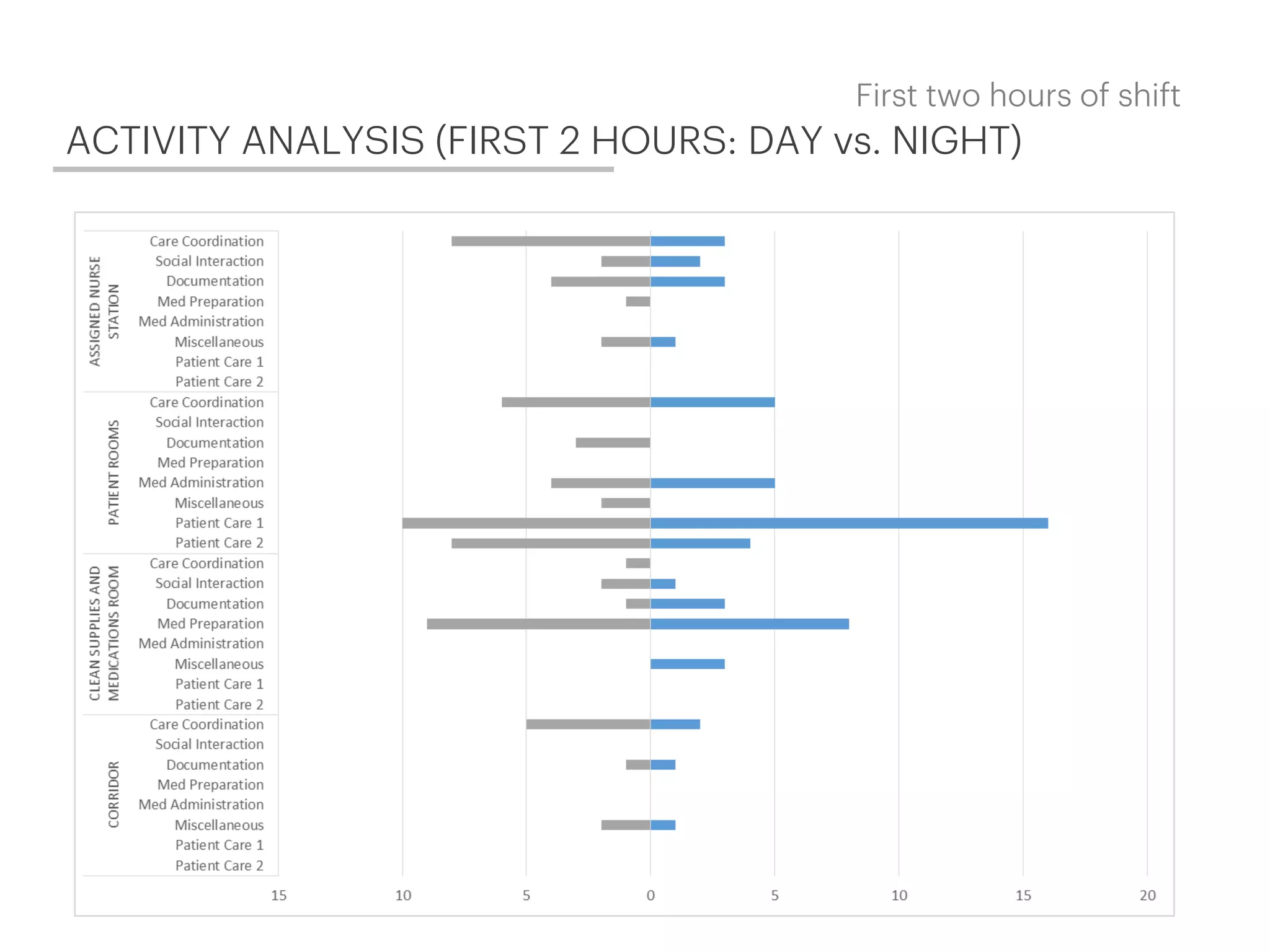
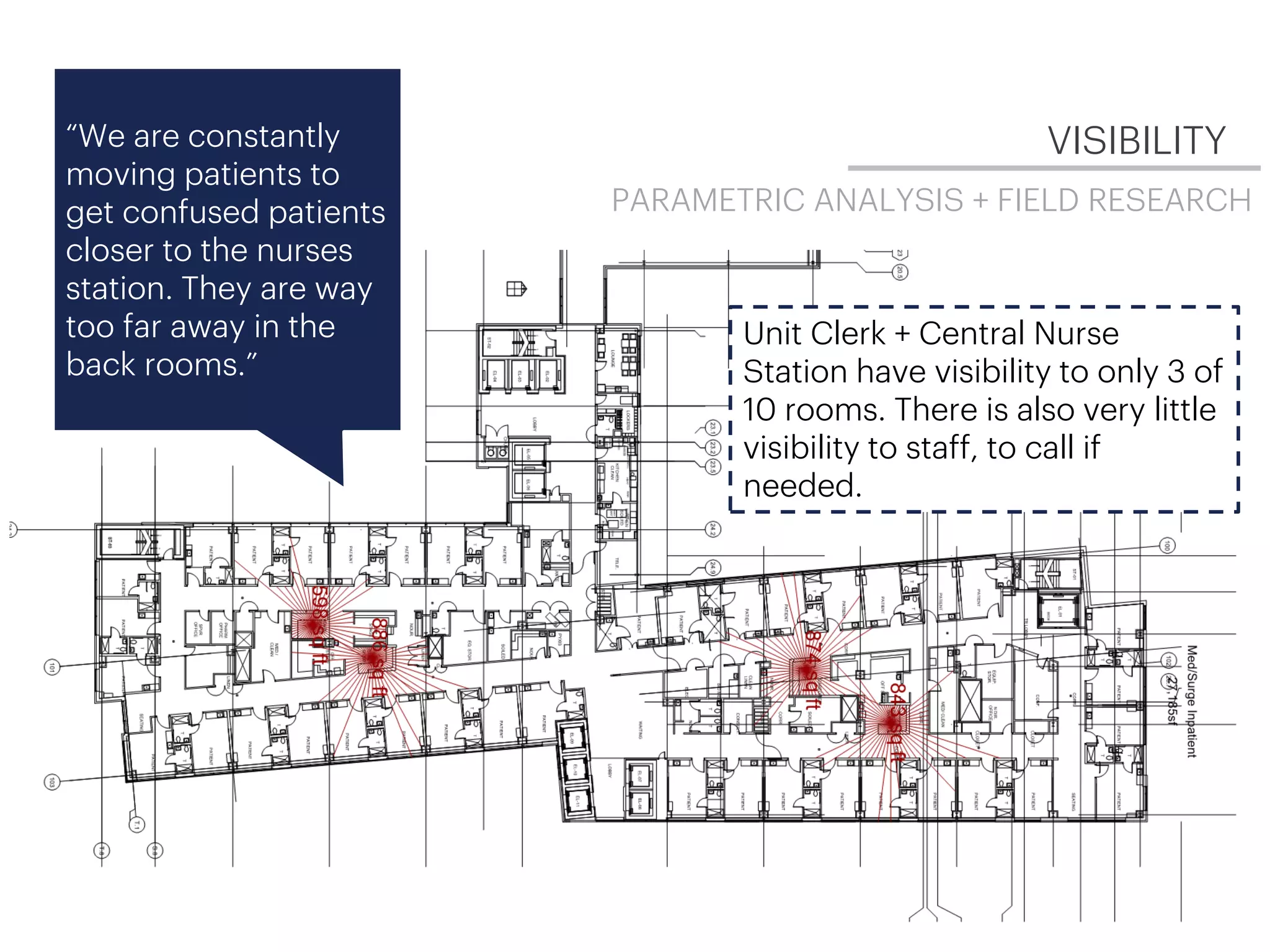
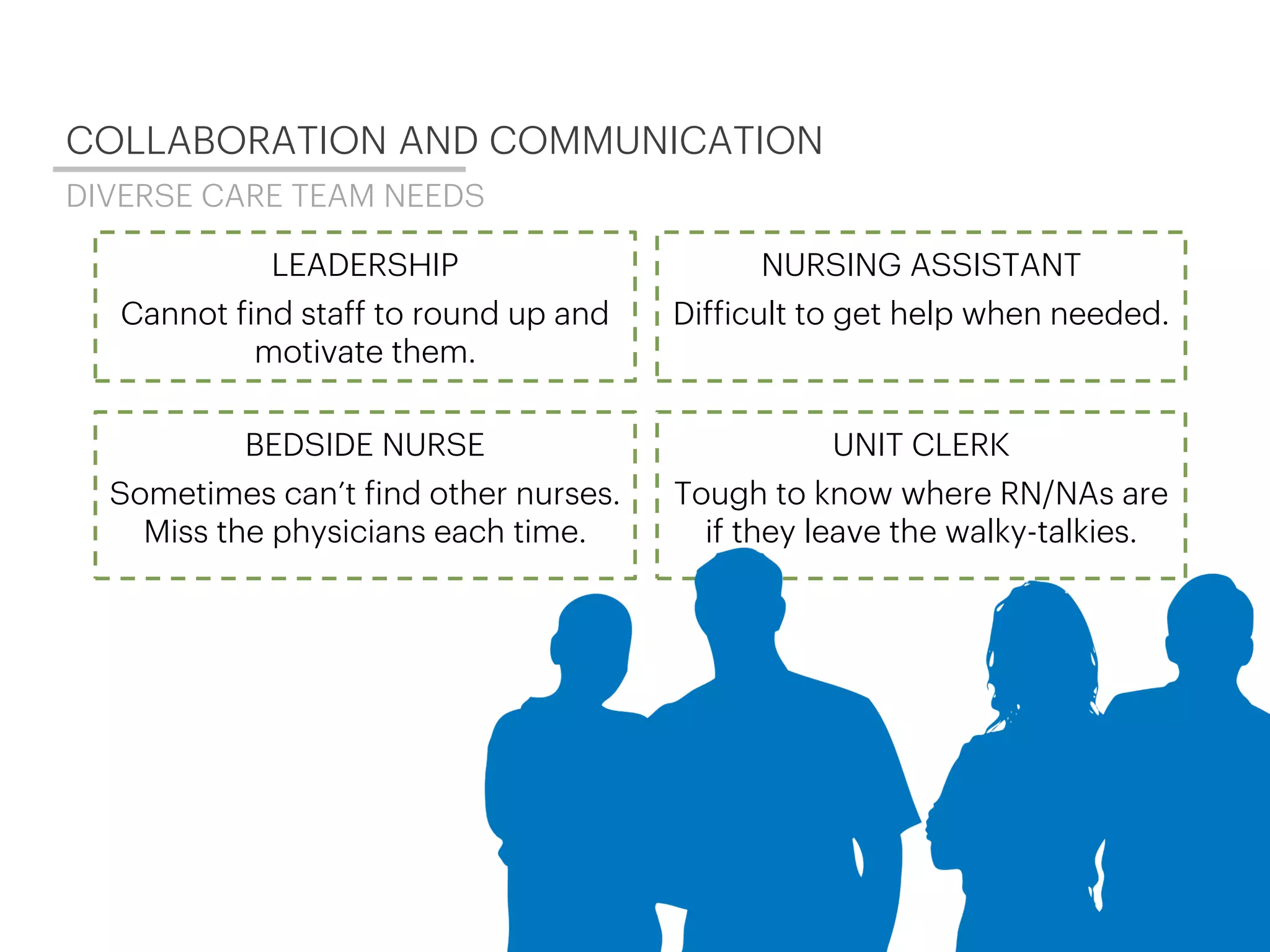
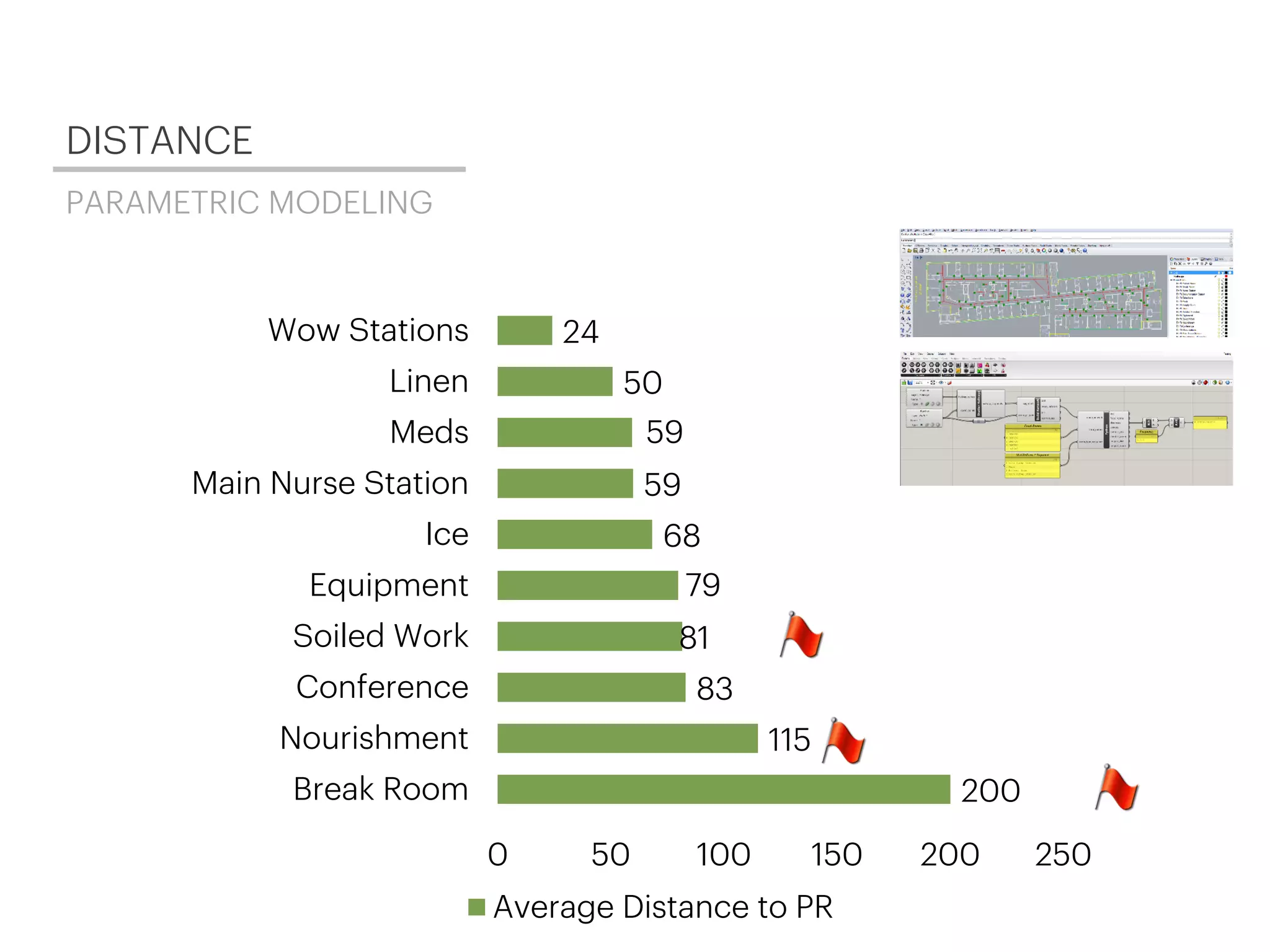
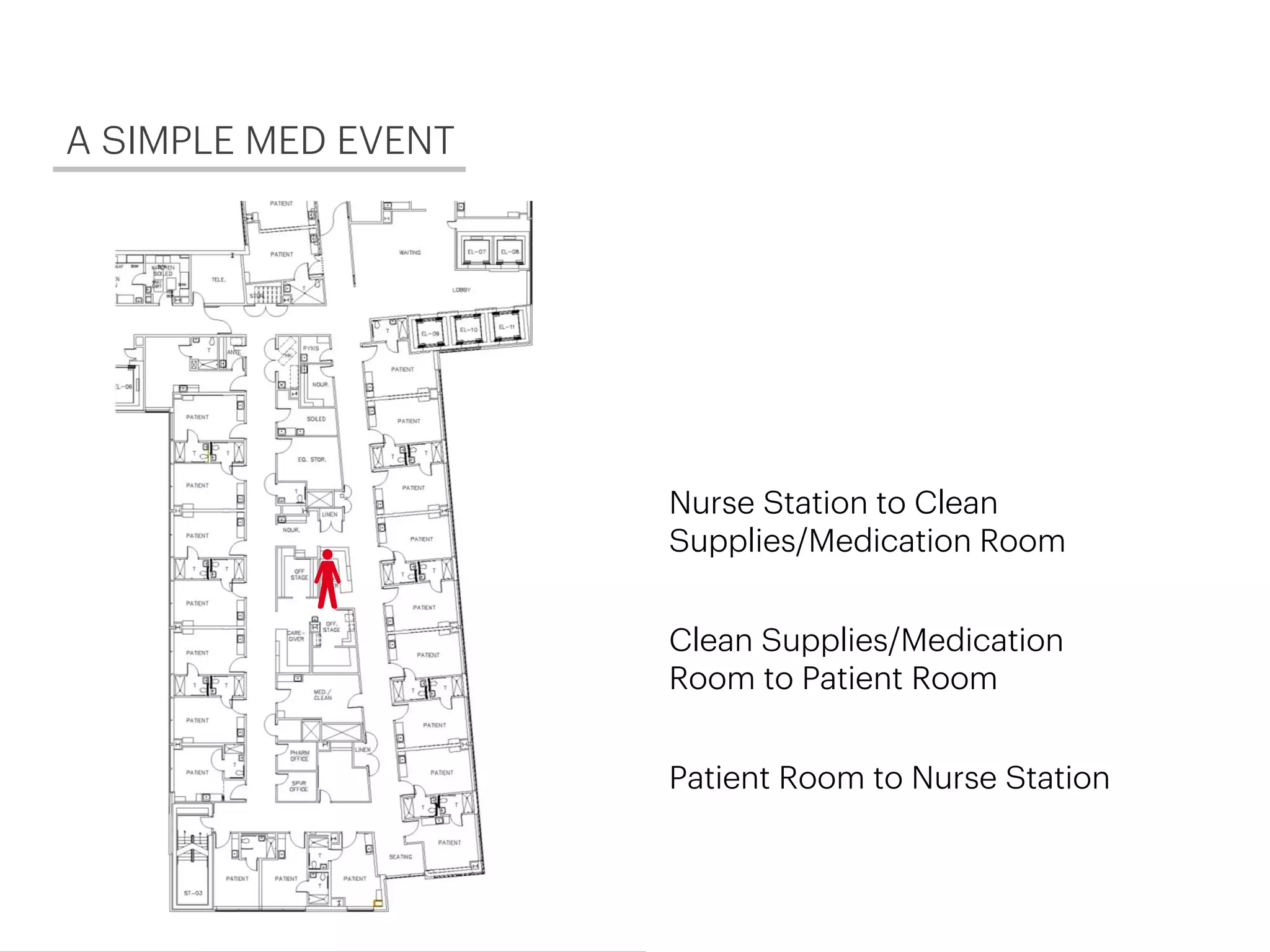
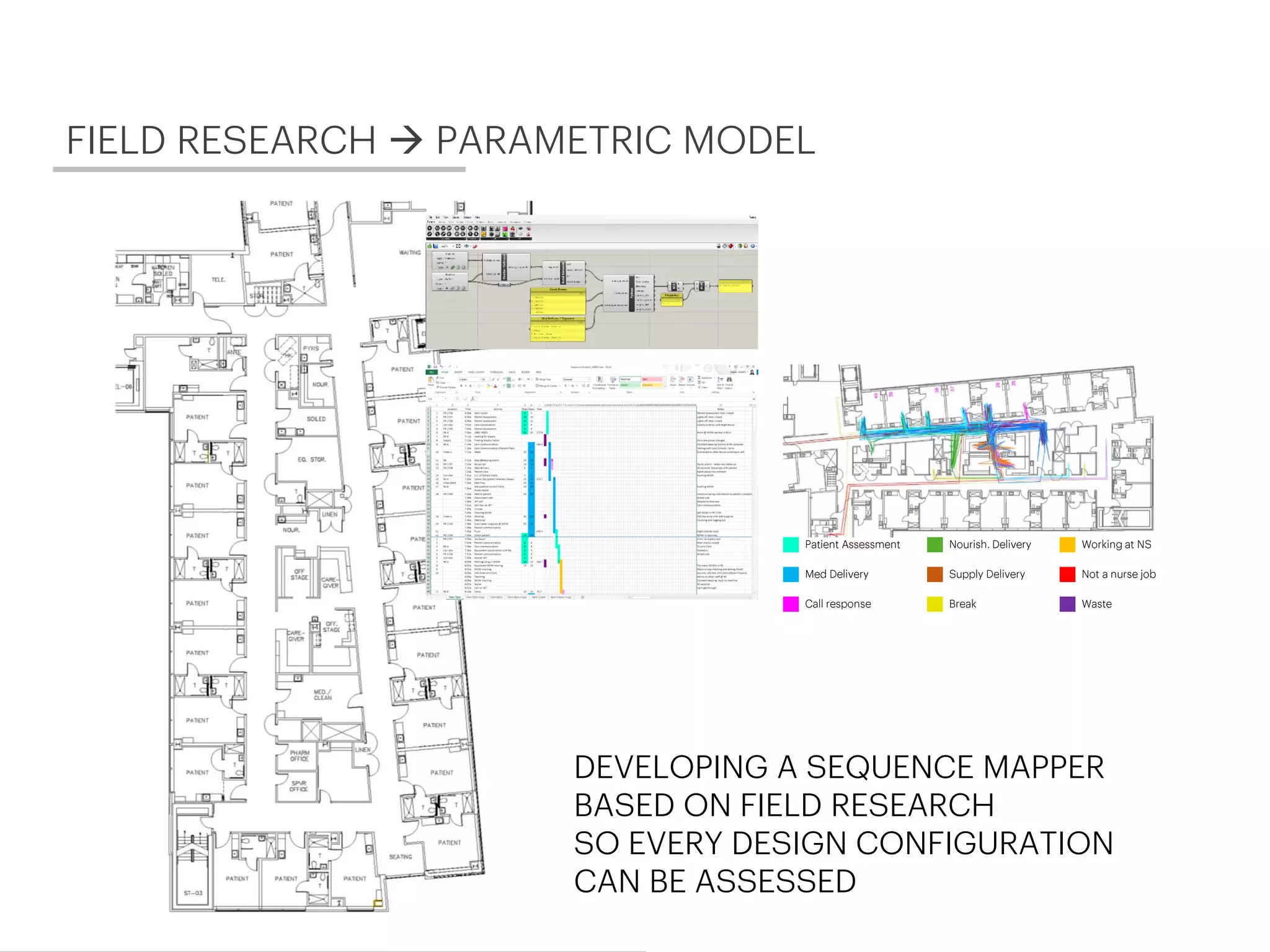
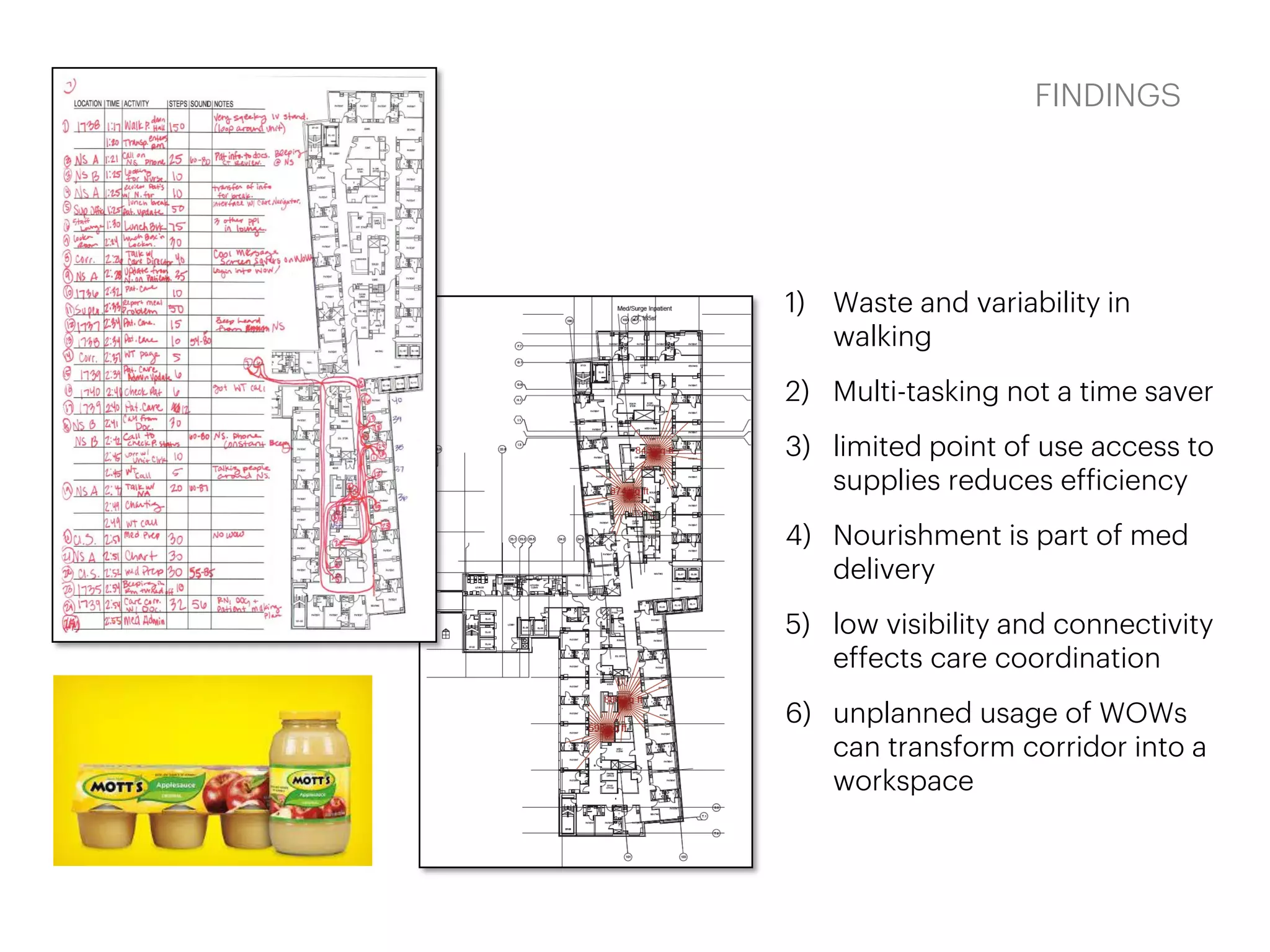
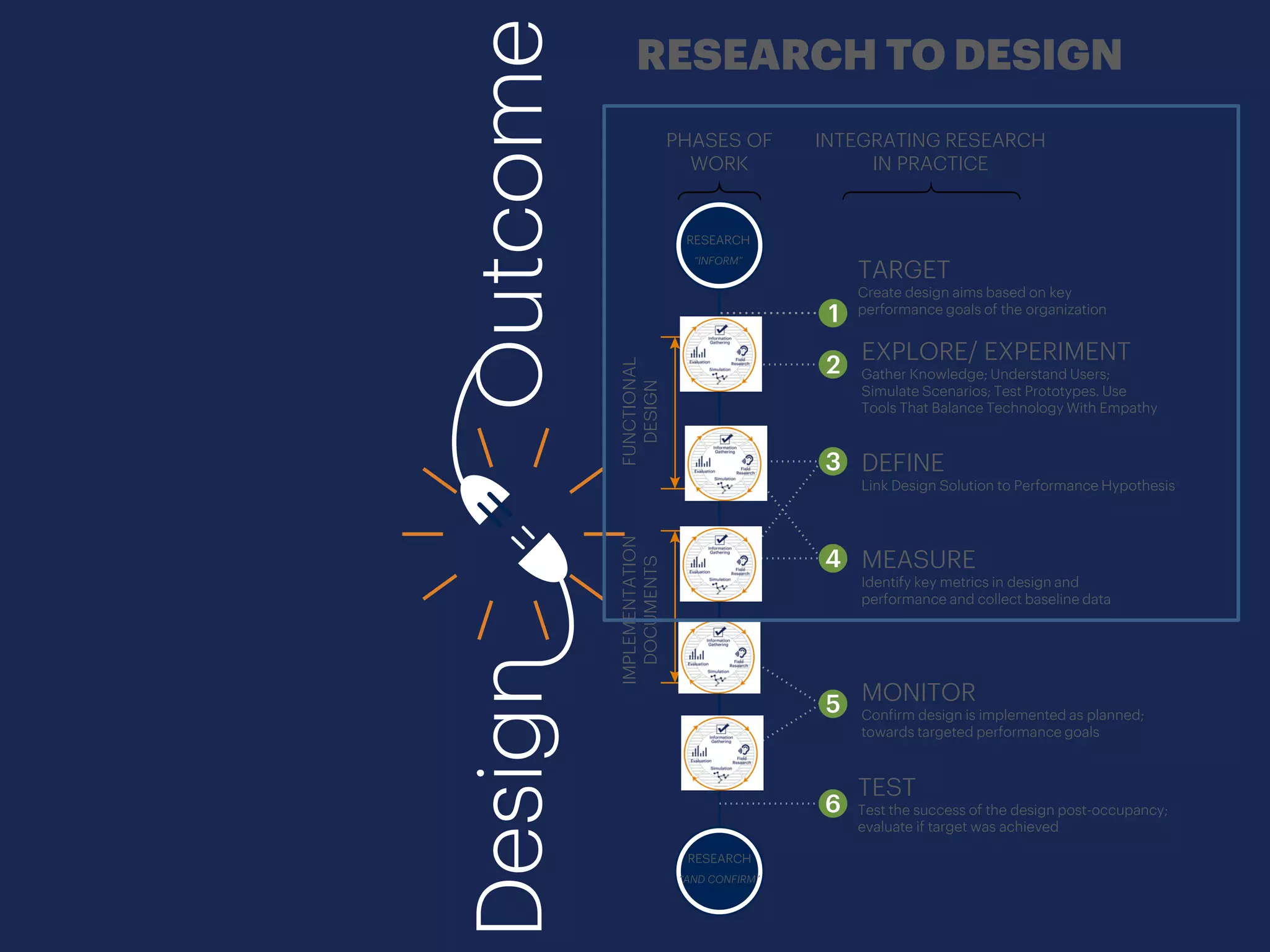
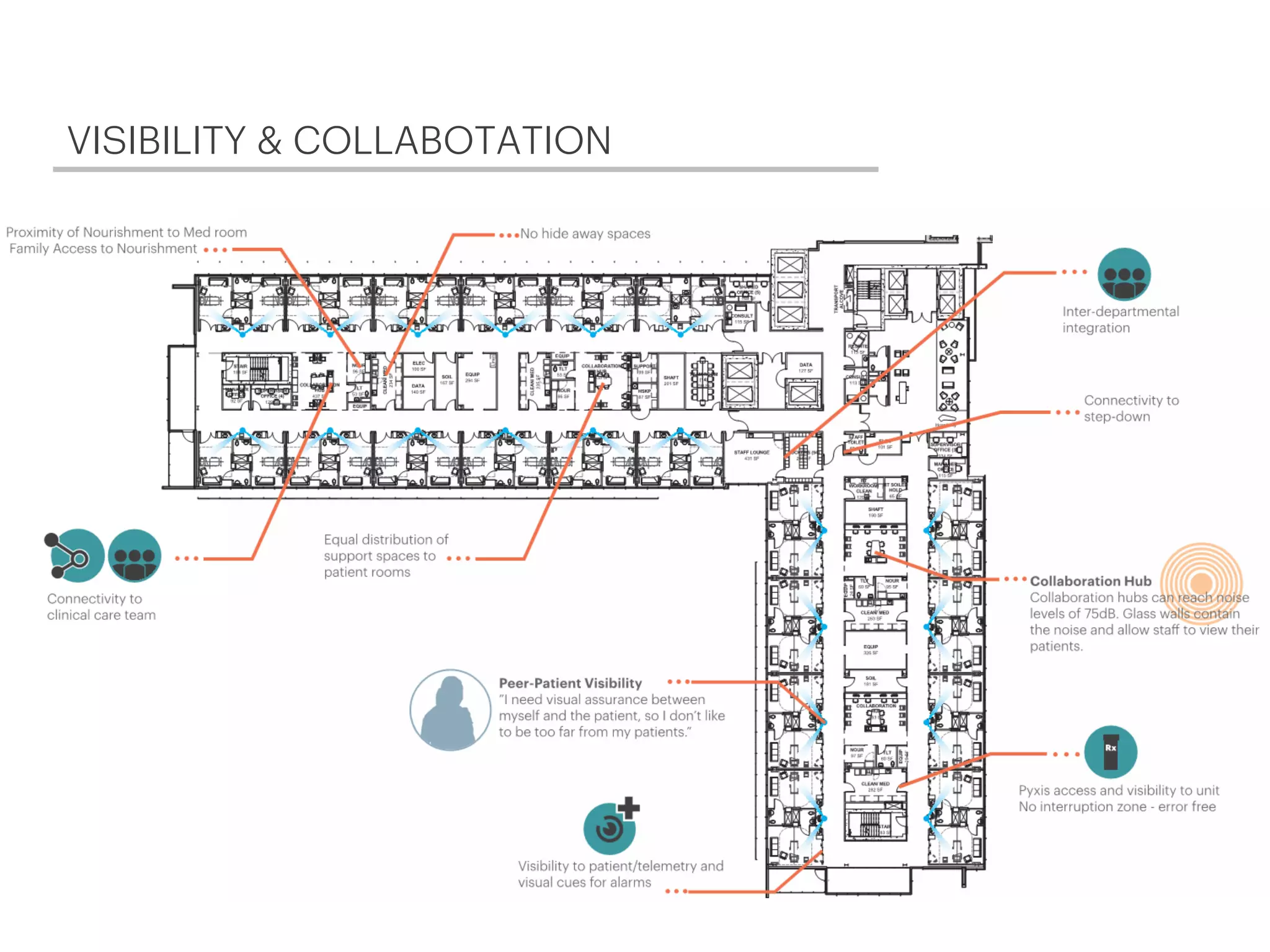
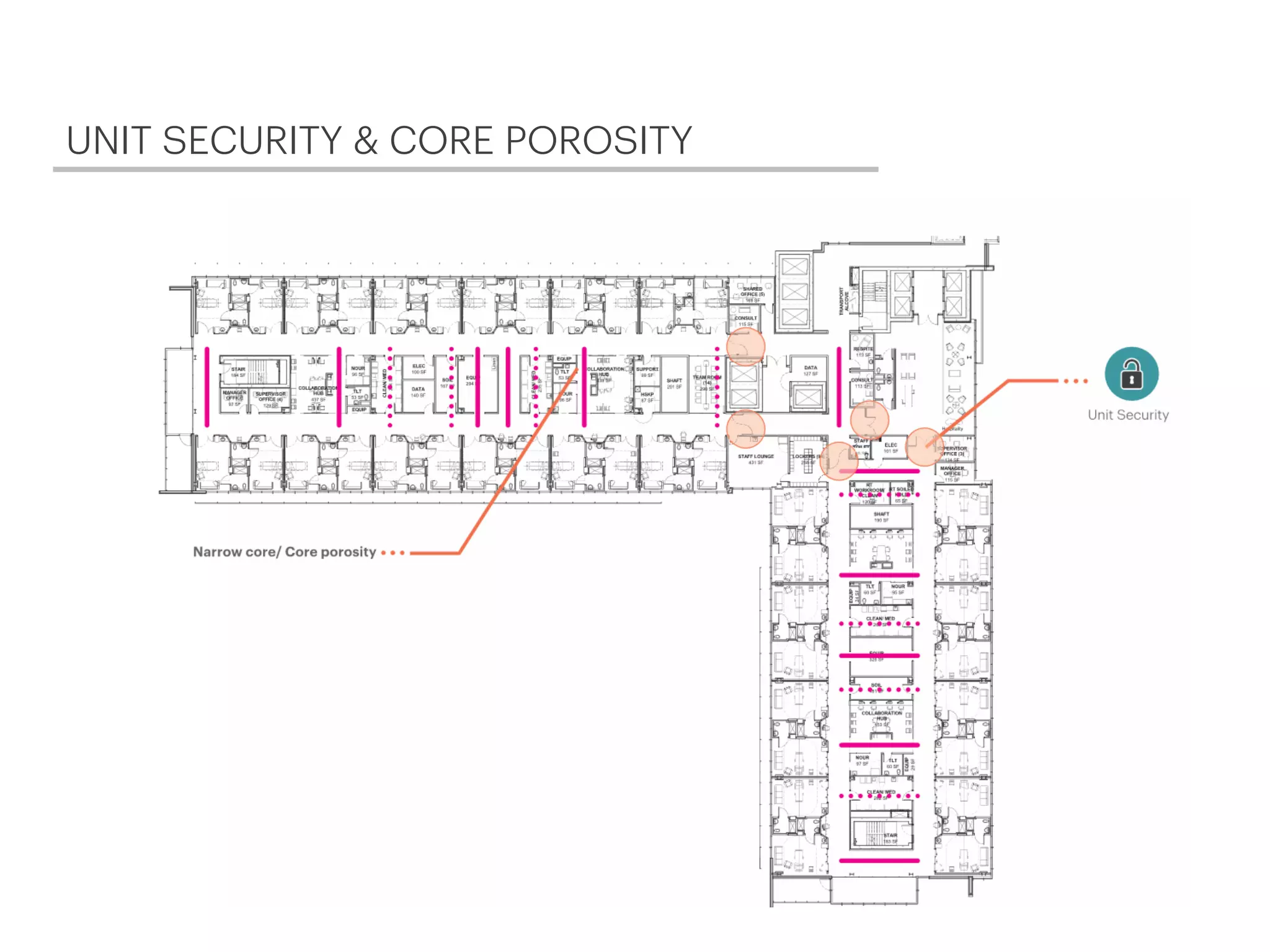
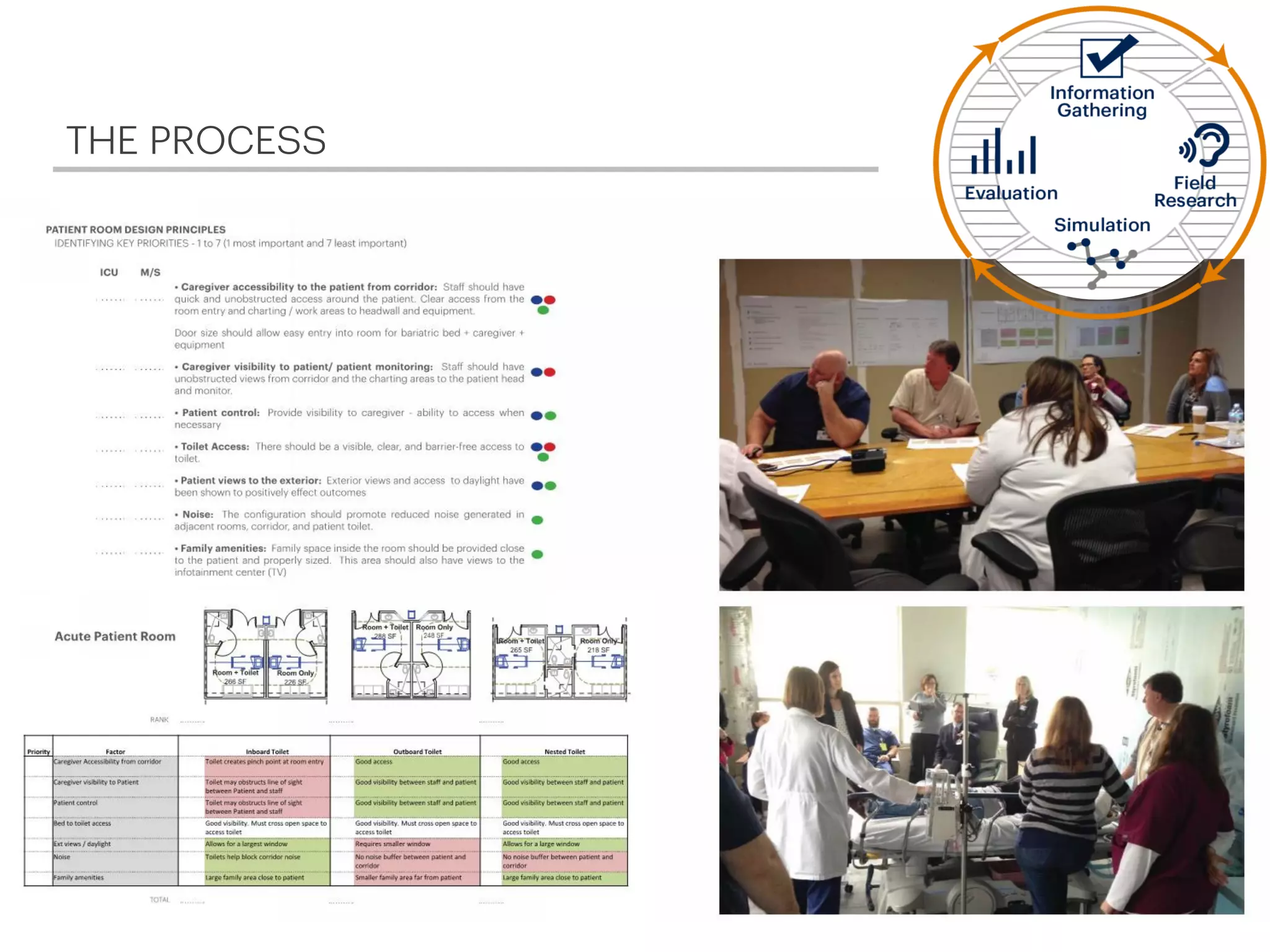
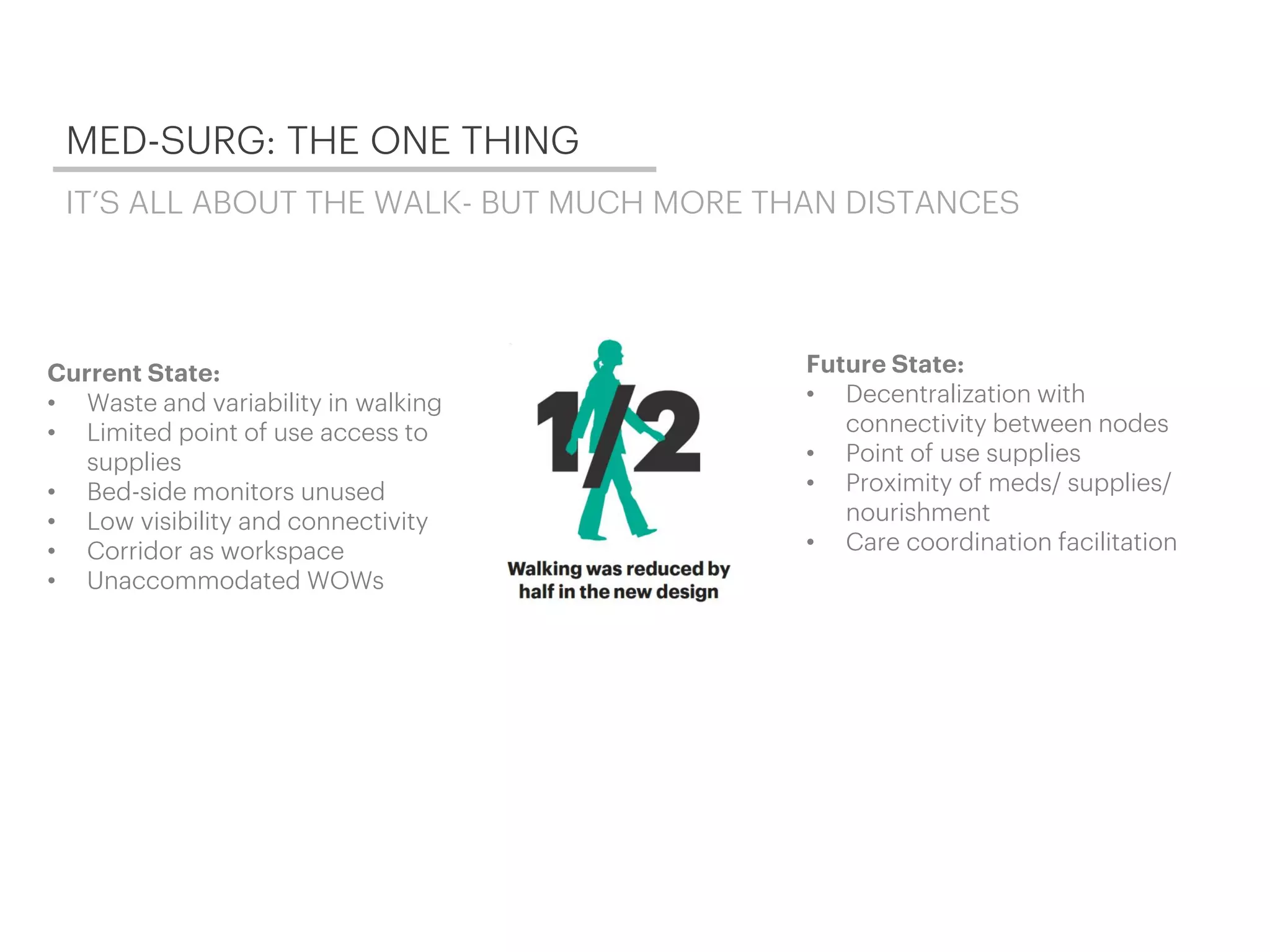
This document discusses how field research and parametric analysis were used to inform the design of a new patient tower for ProMedica Toledo Hospital. Researchers conducted observations and activity analysis of a current med-surg unit to understand issues like wasted walking, limited visibility, and unused space. A parametric model was developed to simulate different design configurations and sequences of staff activities. Key findings included that multi-tasking did not reduce time and point-of-use supplies could improve efficiency. The research helped define targets for the future state design focused on decentralization, proximity of supplies, and improved care coordination.