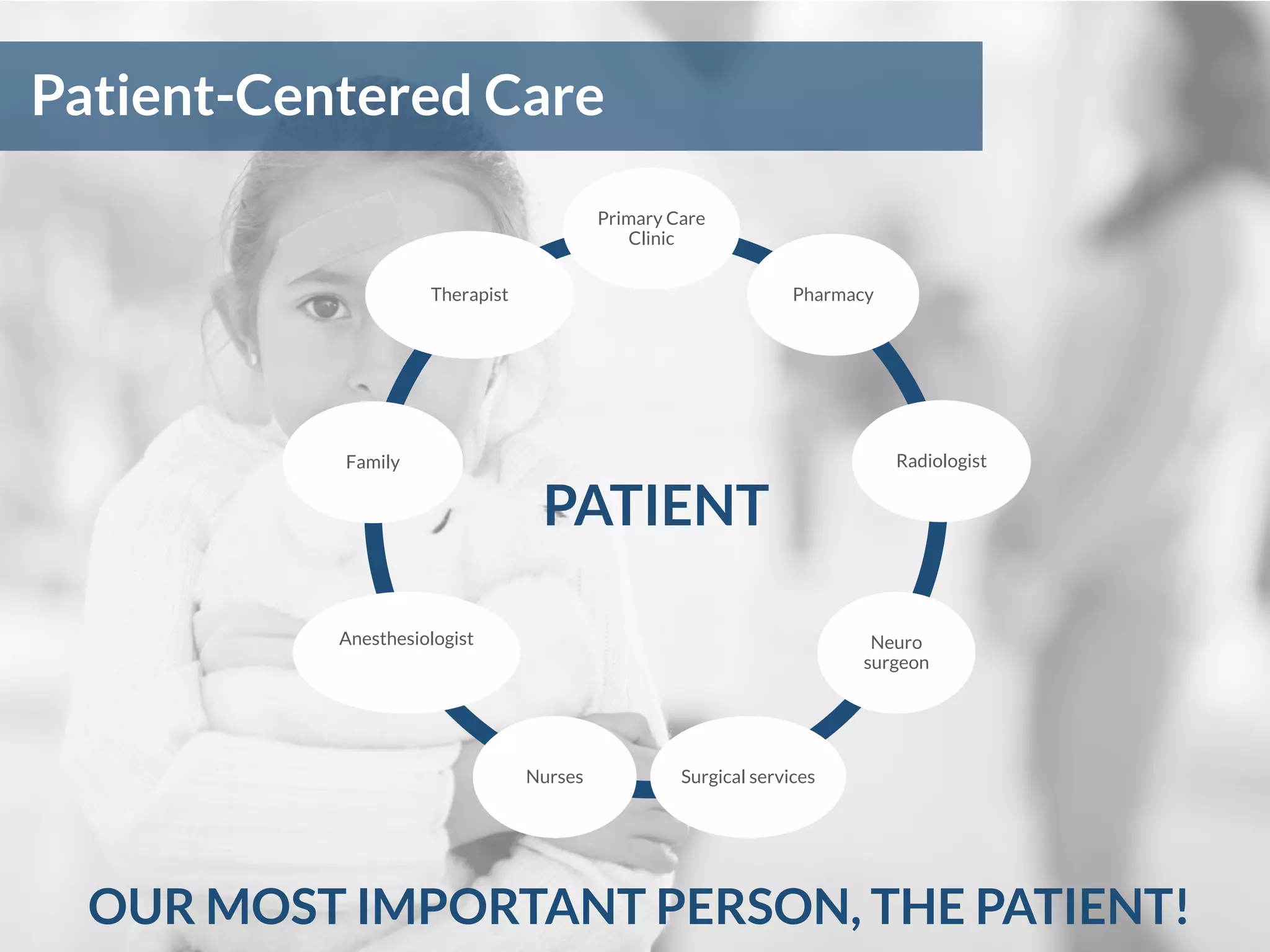
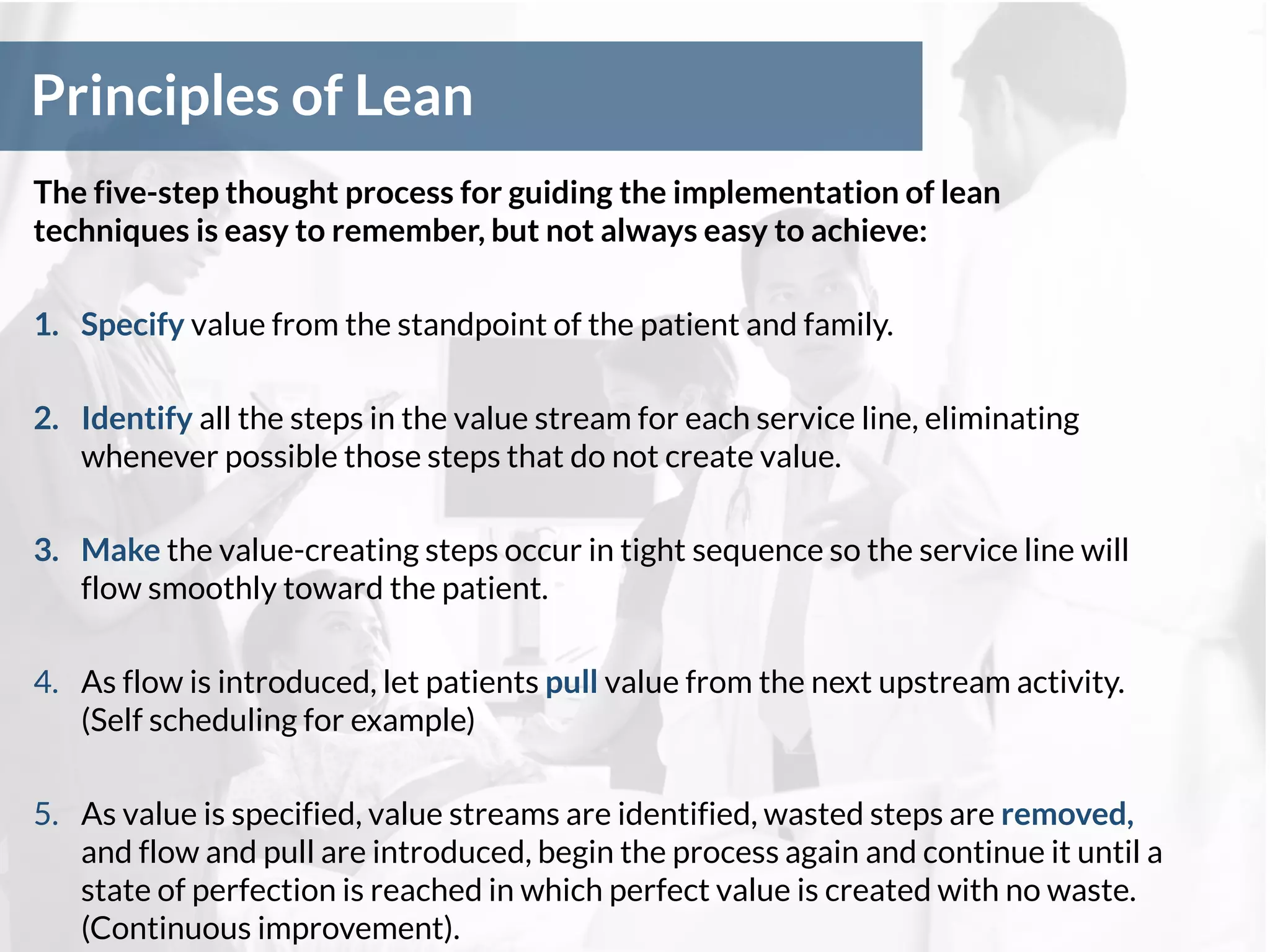
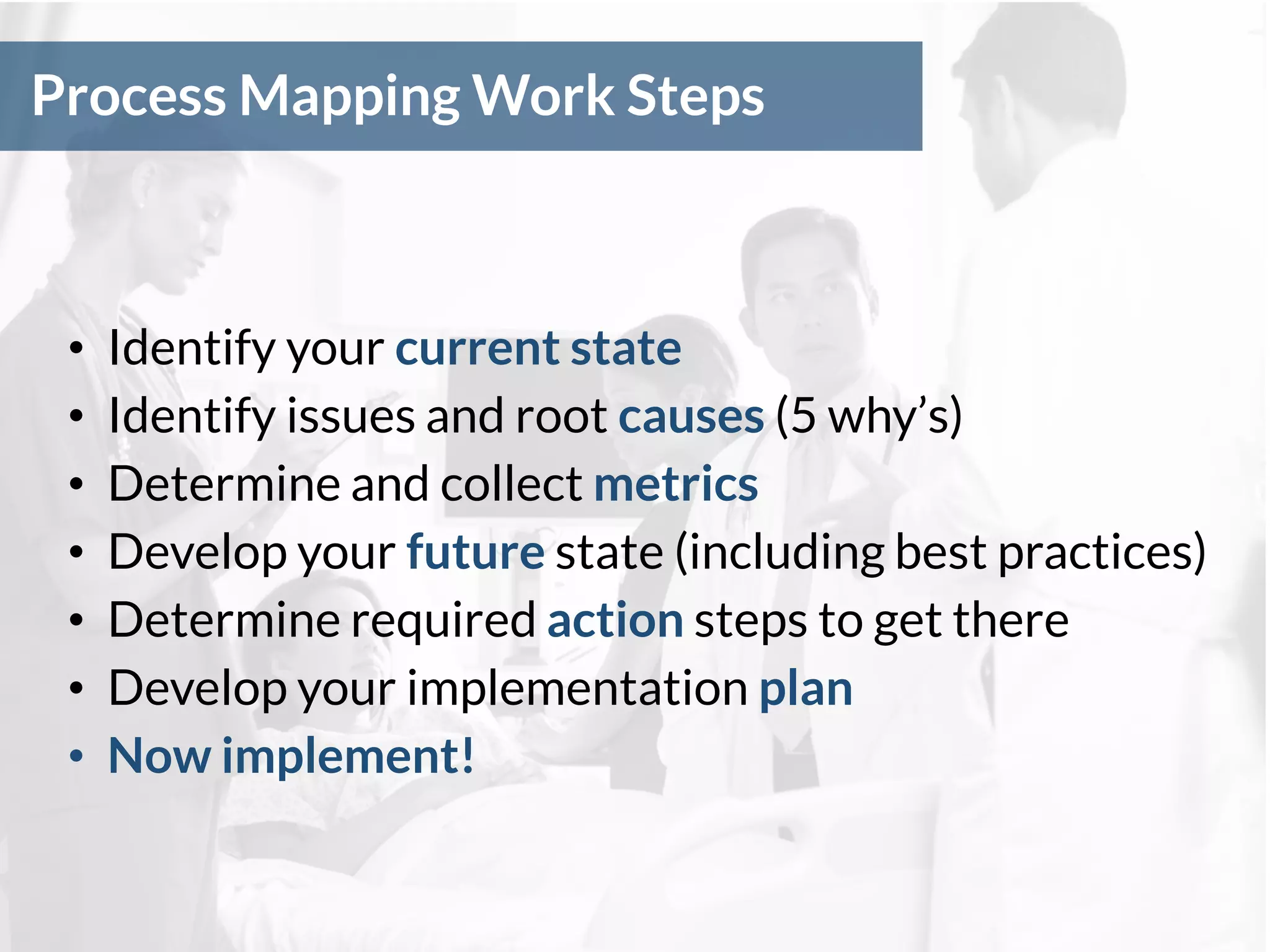
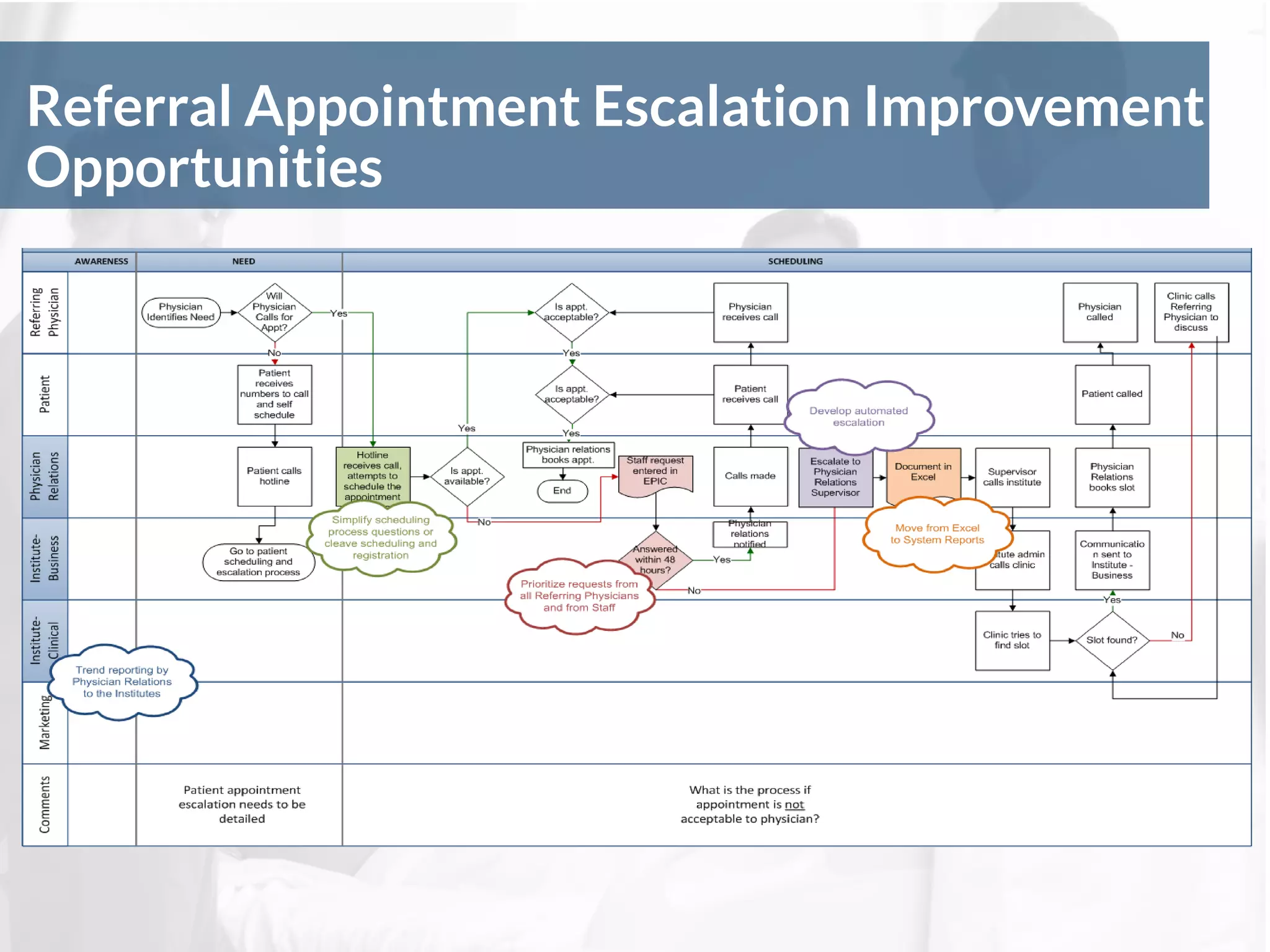
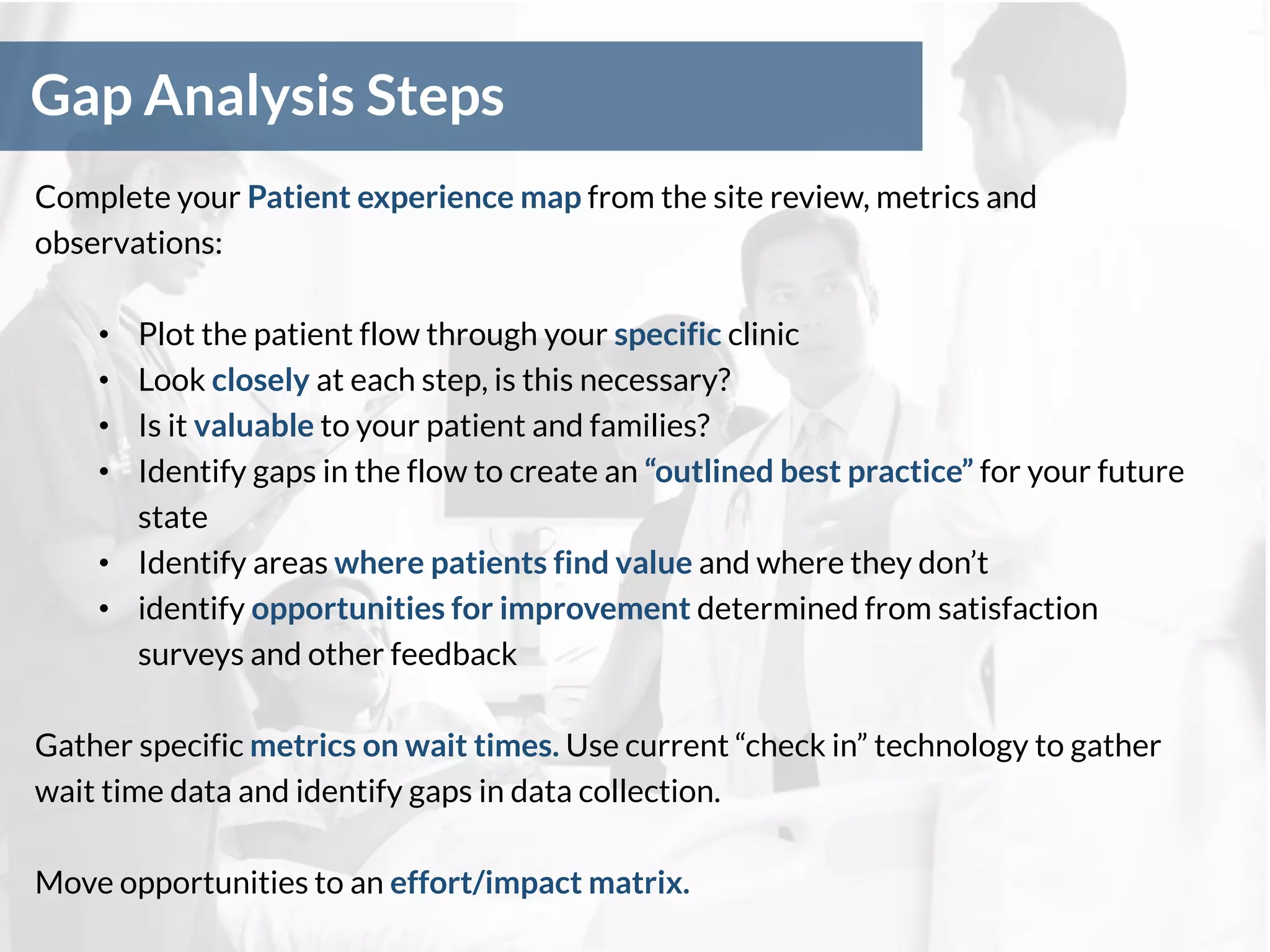
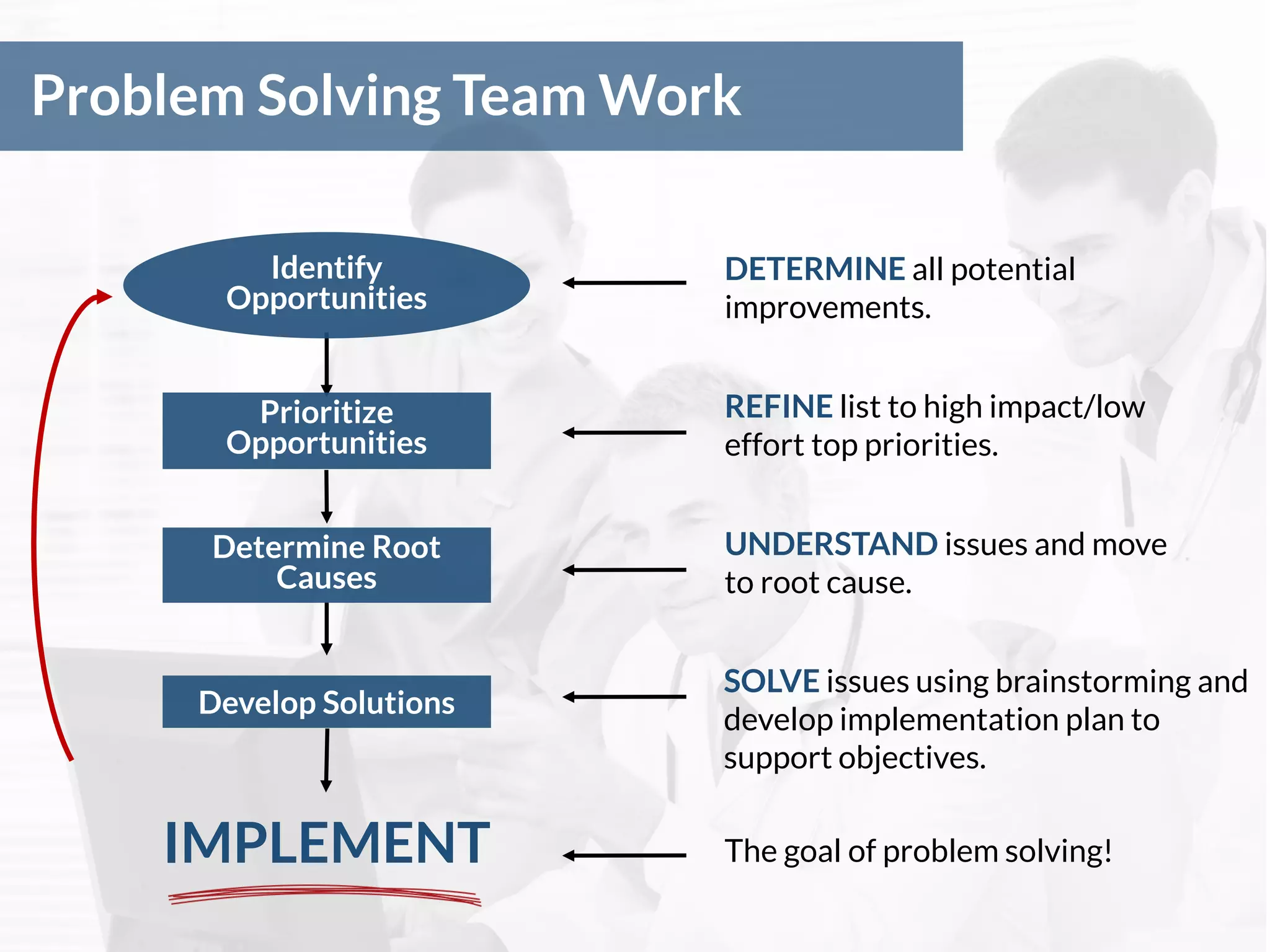
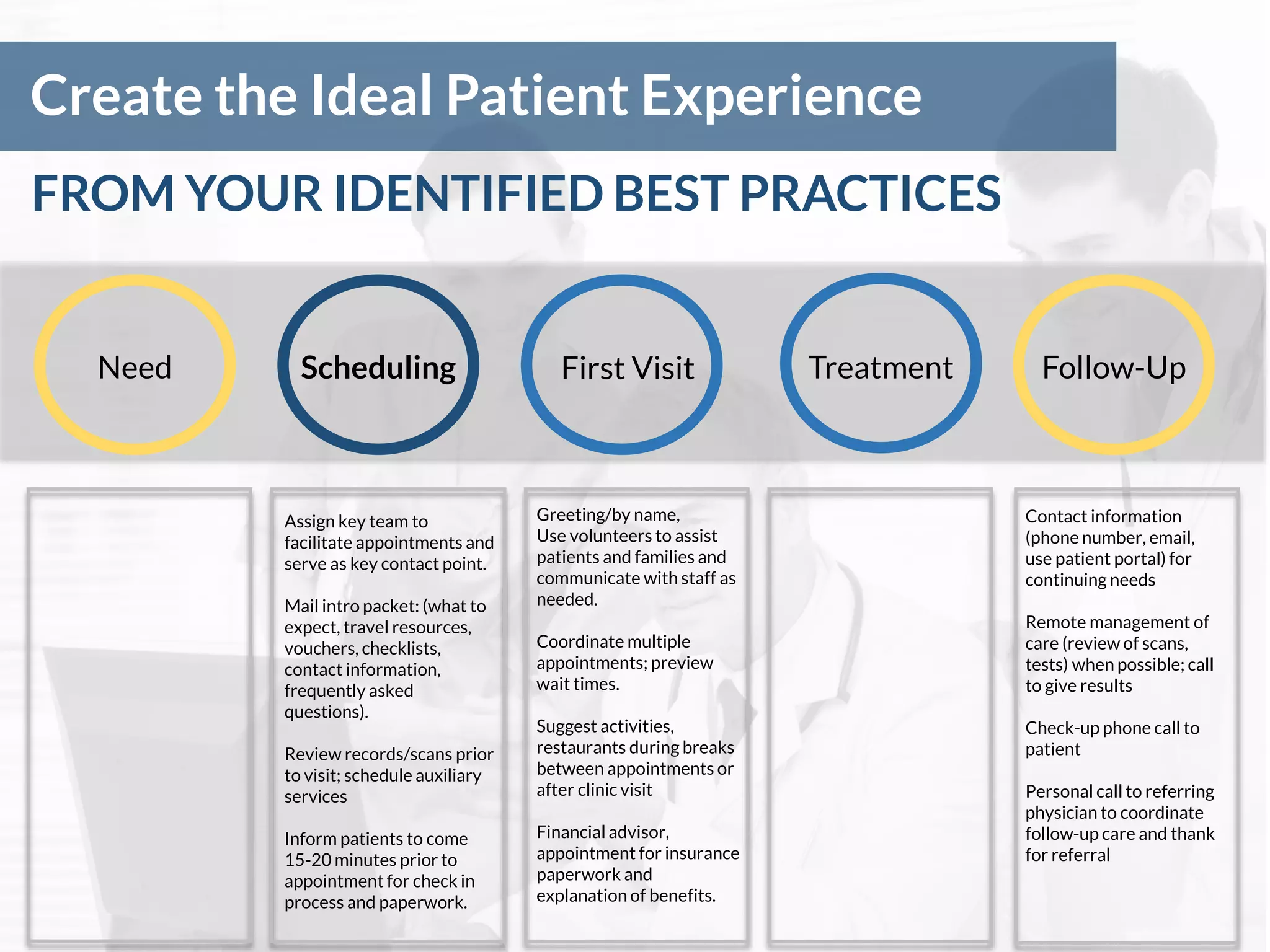
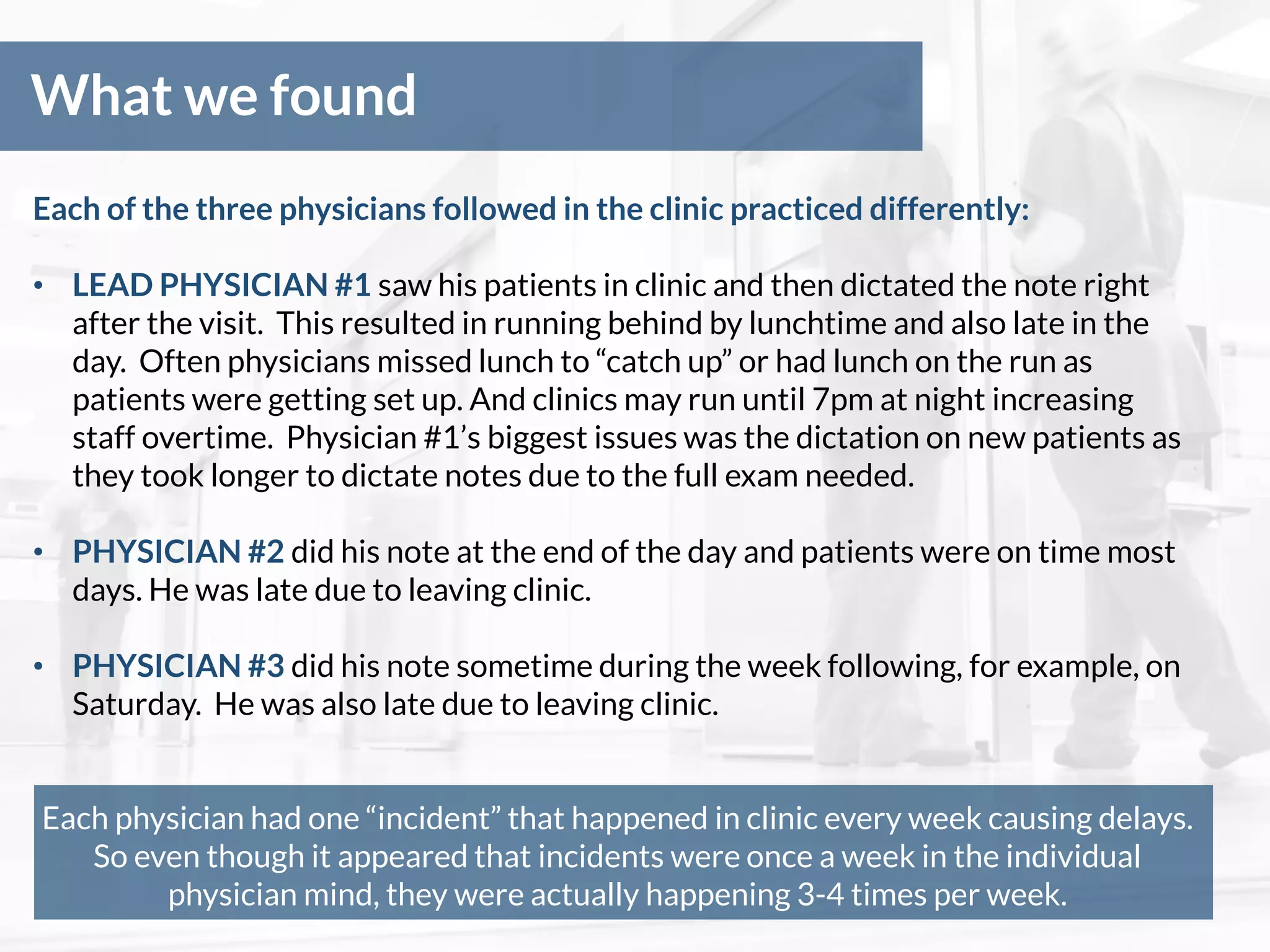
This webinar presentation discussed using Lean healthcare methodologies to improve the patient experience. It began with housekeeping items about the webinar format and then provided information about the speakers' backgrounds working with major healthcare institutions. The presentation objectives were to understand the difference between emotional and functional needs, learn some Lean techniques that can be used in clinics, and identify tools for future efficiency projects. Various Lean concepts and methods were then explained like process mapping, identifying waste, and creating ideal patient flows. An example was provided of how these techniques were used to improve wait times in a thoracic surgery clinic by changing a physician's schedule and adding a floating physician role. The results were improved on-time performance and higher patient satisfaction scores.