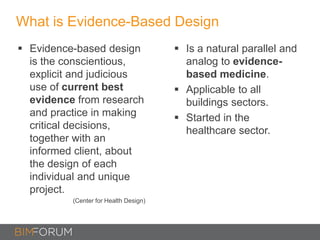
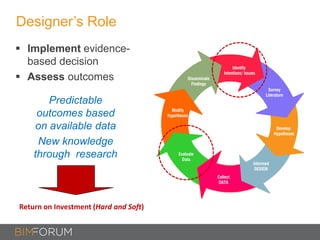
1) Evidence-based design (EBD) emerged in healthcare to improve safety and outcomes using research-informed design decisions.
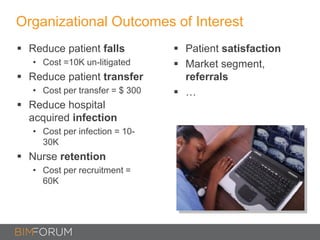
2) Studies found EBD strategies like decentralized nursing units reduced patient falls by 75% and transfers by 90%.
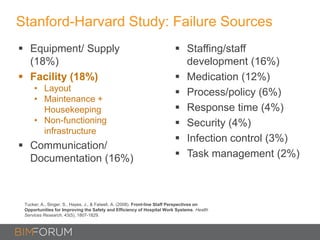
3) Other research linked factors like patient visibility and private rooms to lower mortality and infection risk.
4) For BIM to be truly evidence-based, it needs an empirical evidence base from built project performance and linkage to organizational goals, not just cost savings.