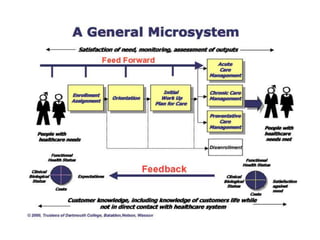
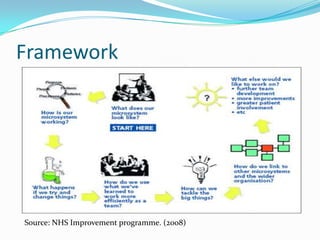
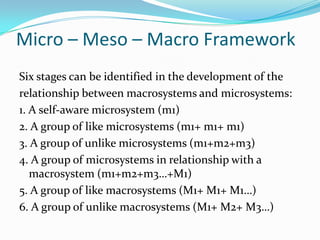
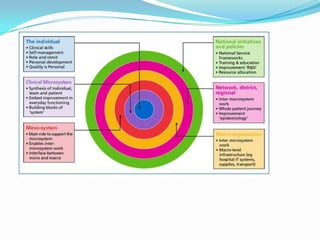
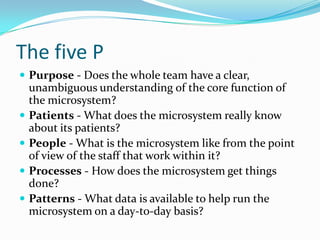
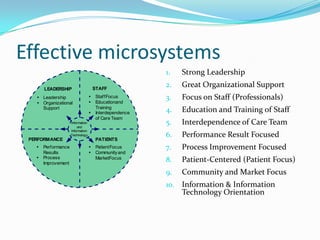
This document discusses clinical microsystems, which are small groups of healthcare professionals and staff who work together to provide care for a defined patient population. A clinical microsystem has shared goals, processes, an information environment, and is responsible for performance outcomes. The document outlines the key components of a microsystem, including its purpose, patients, staff, processes, and patterns. It also discusses how microsystems relate to larger macrosystems in a healthcare organization and the benefits of using a microsystem approach to improve care quality, safety, and staff experience.