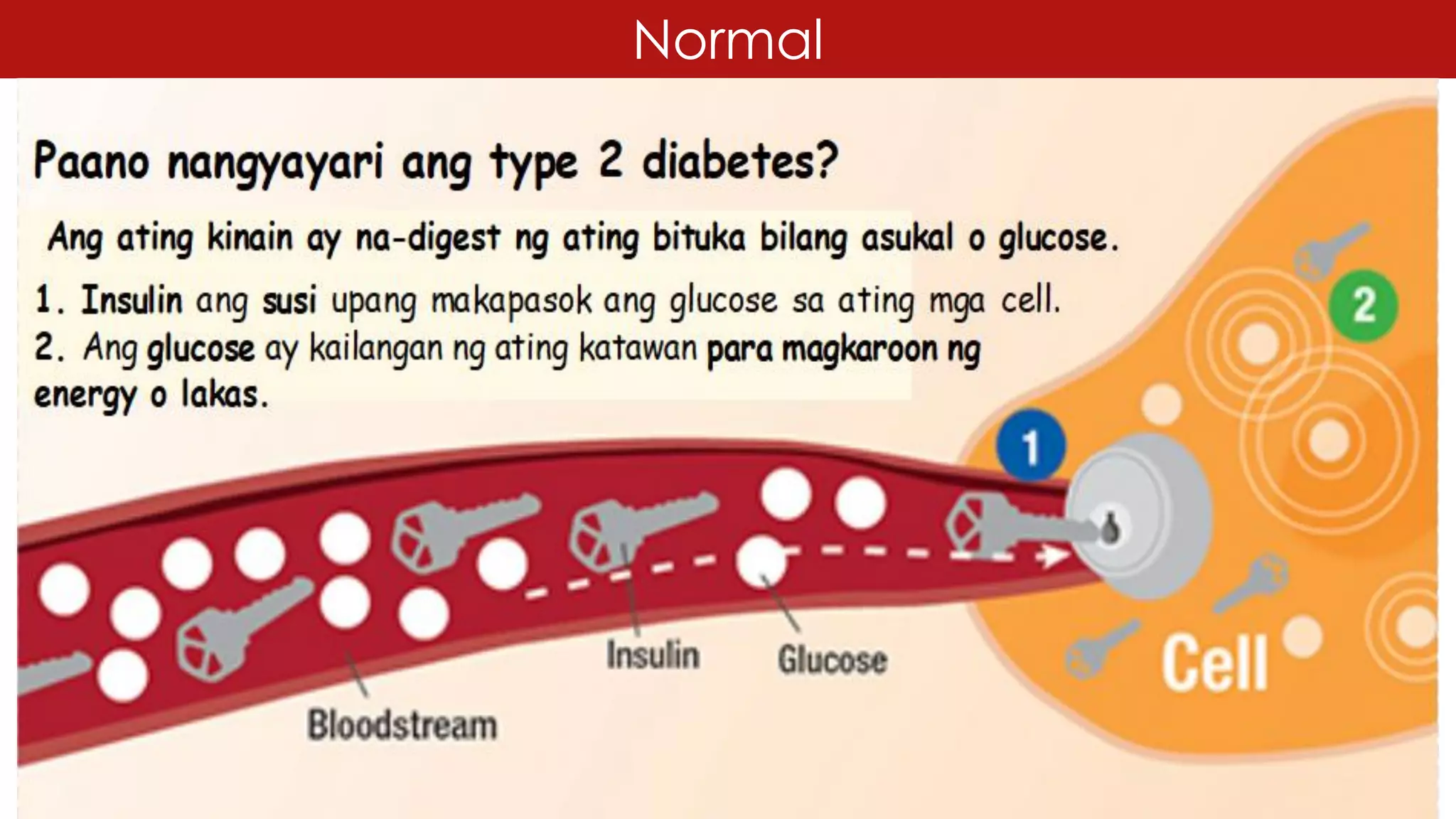
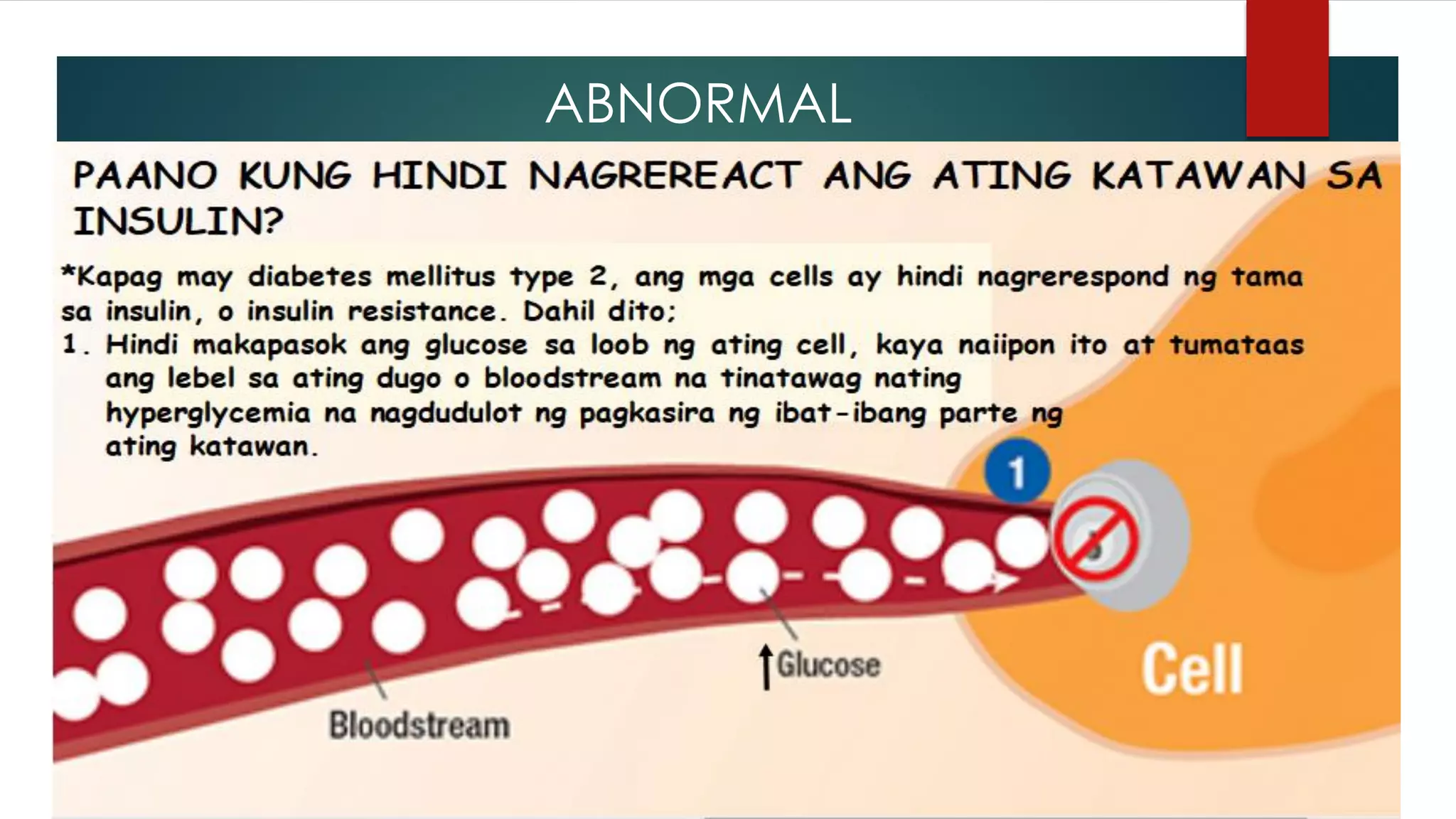
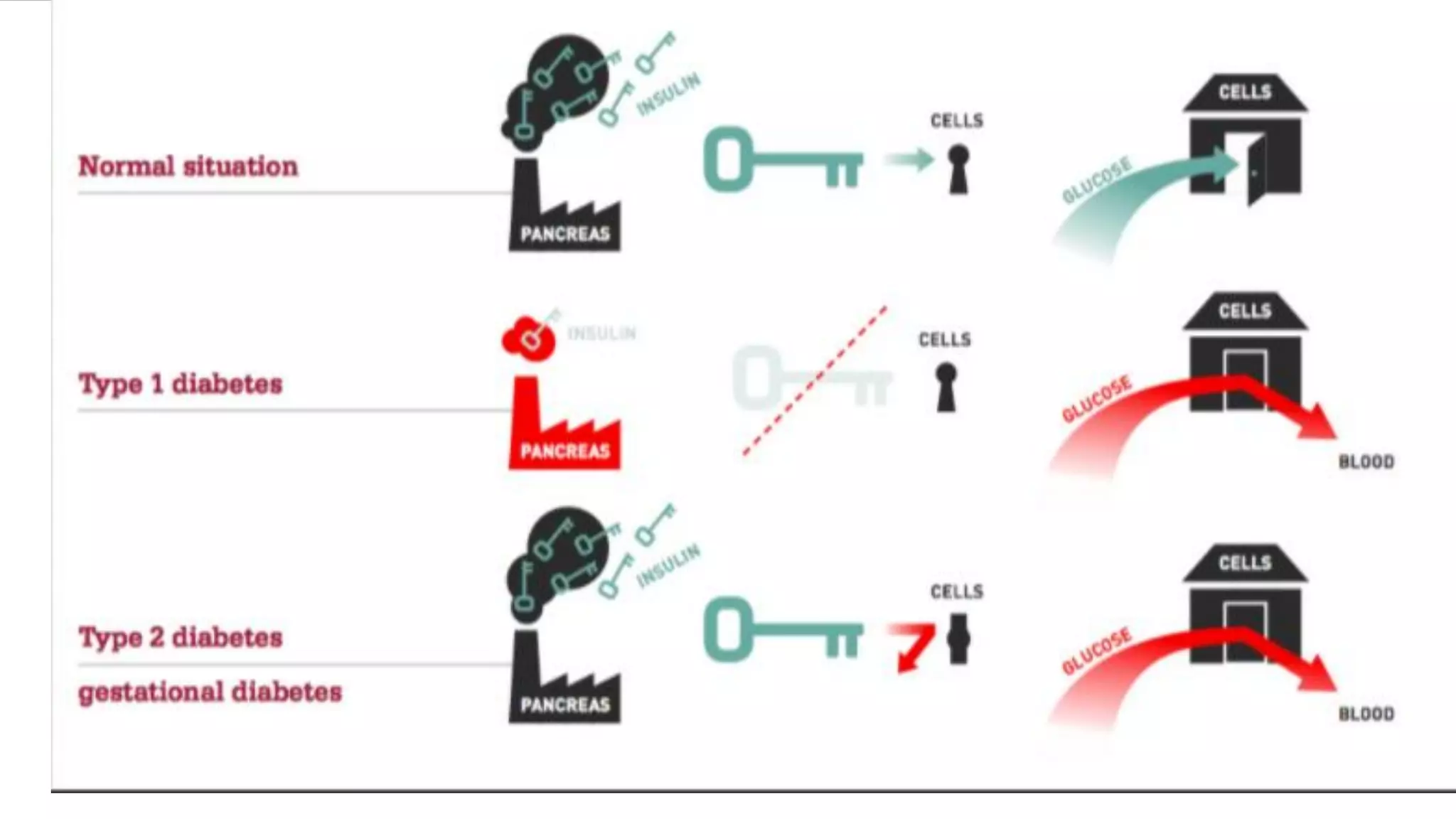
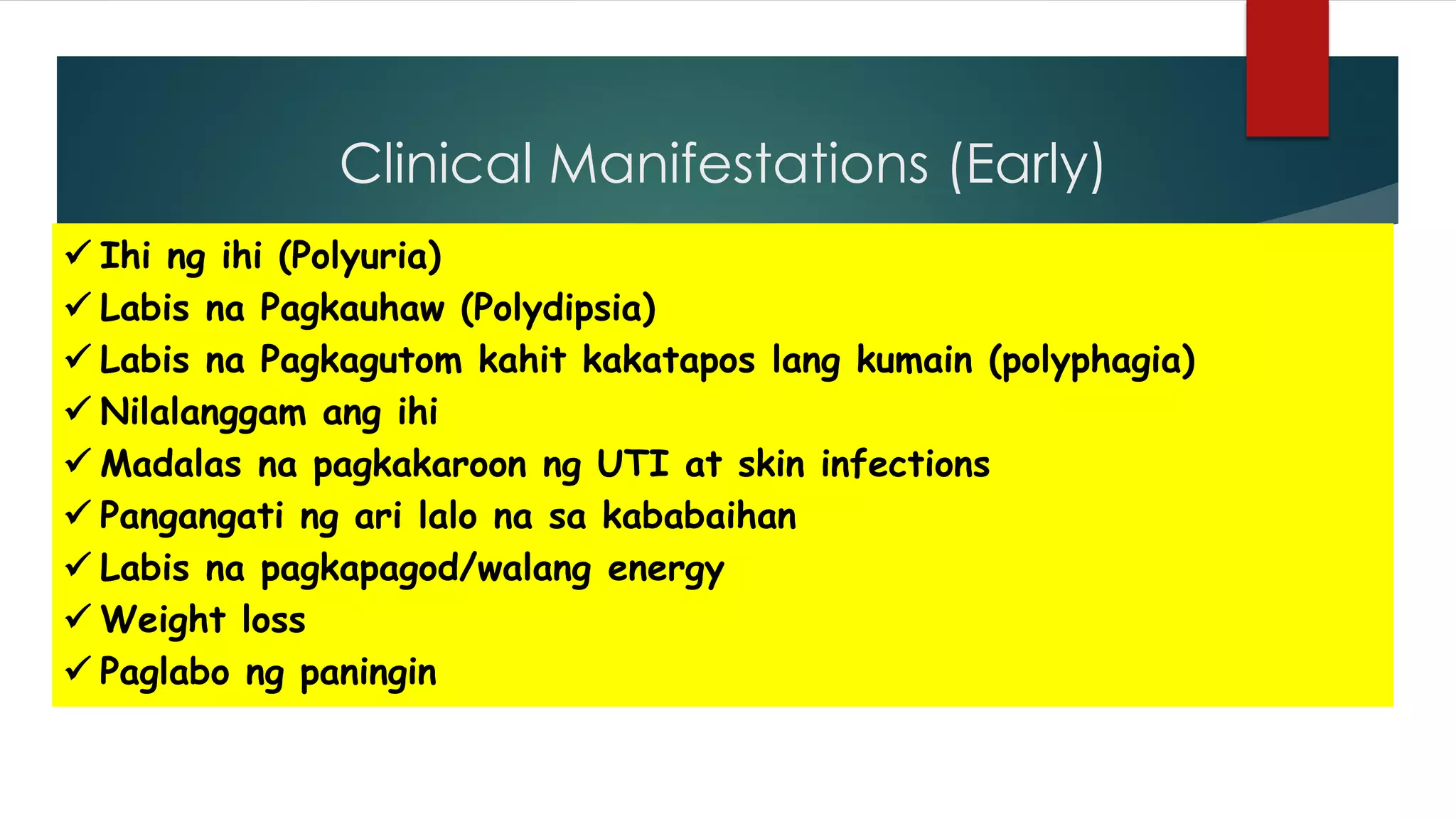
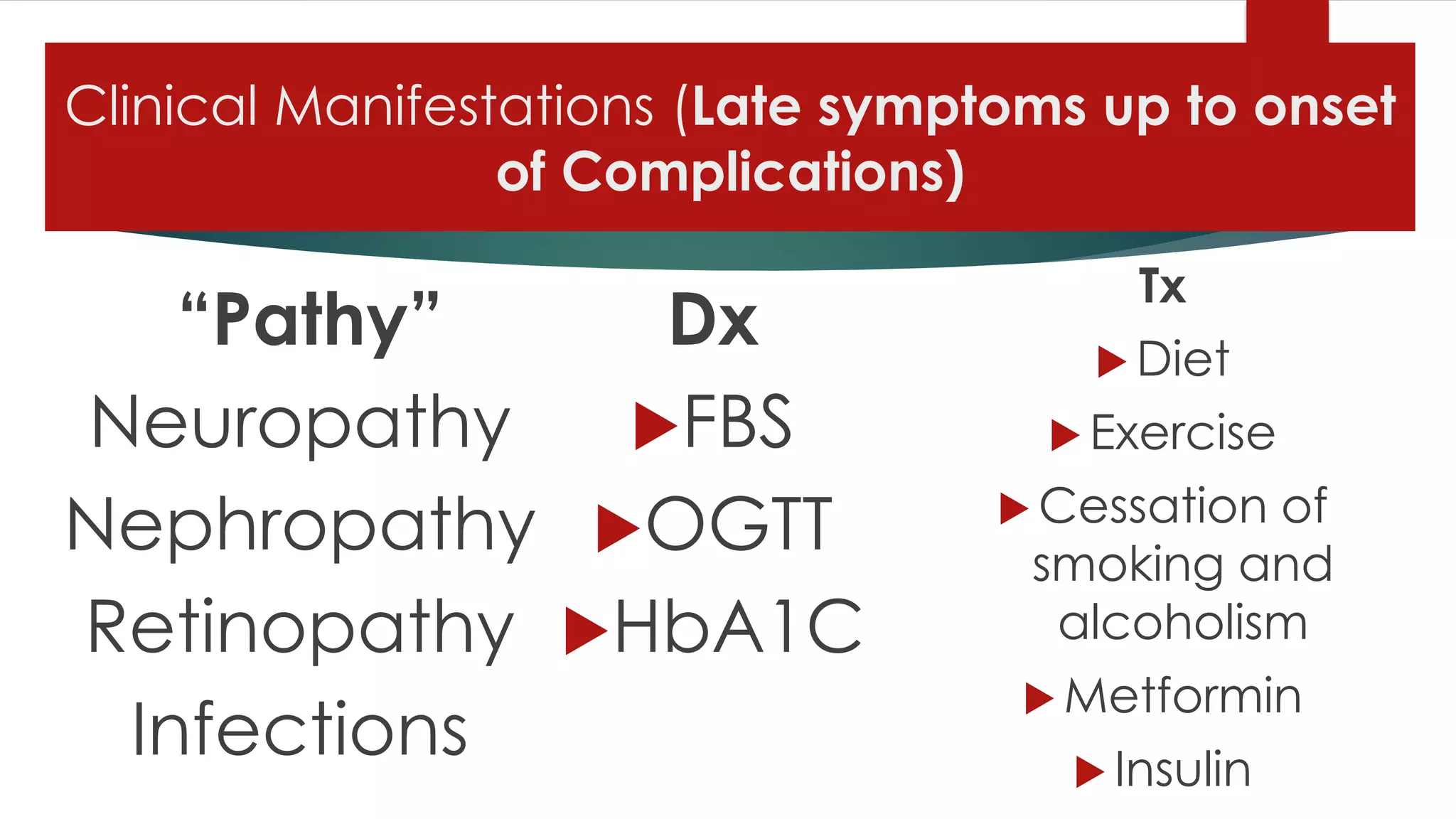
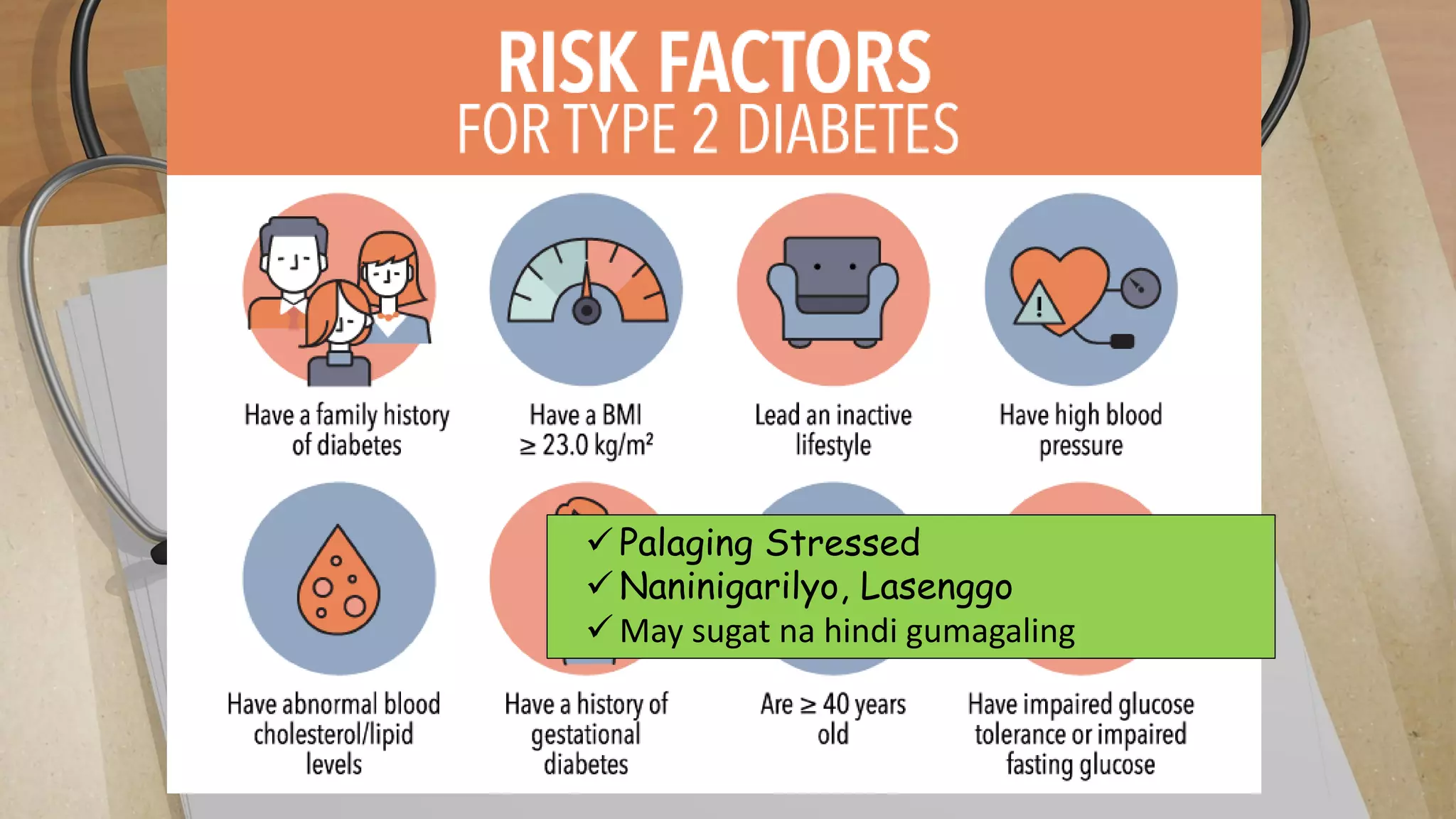
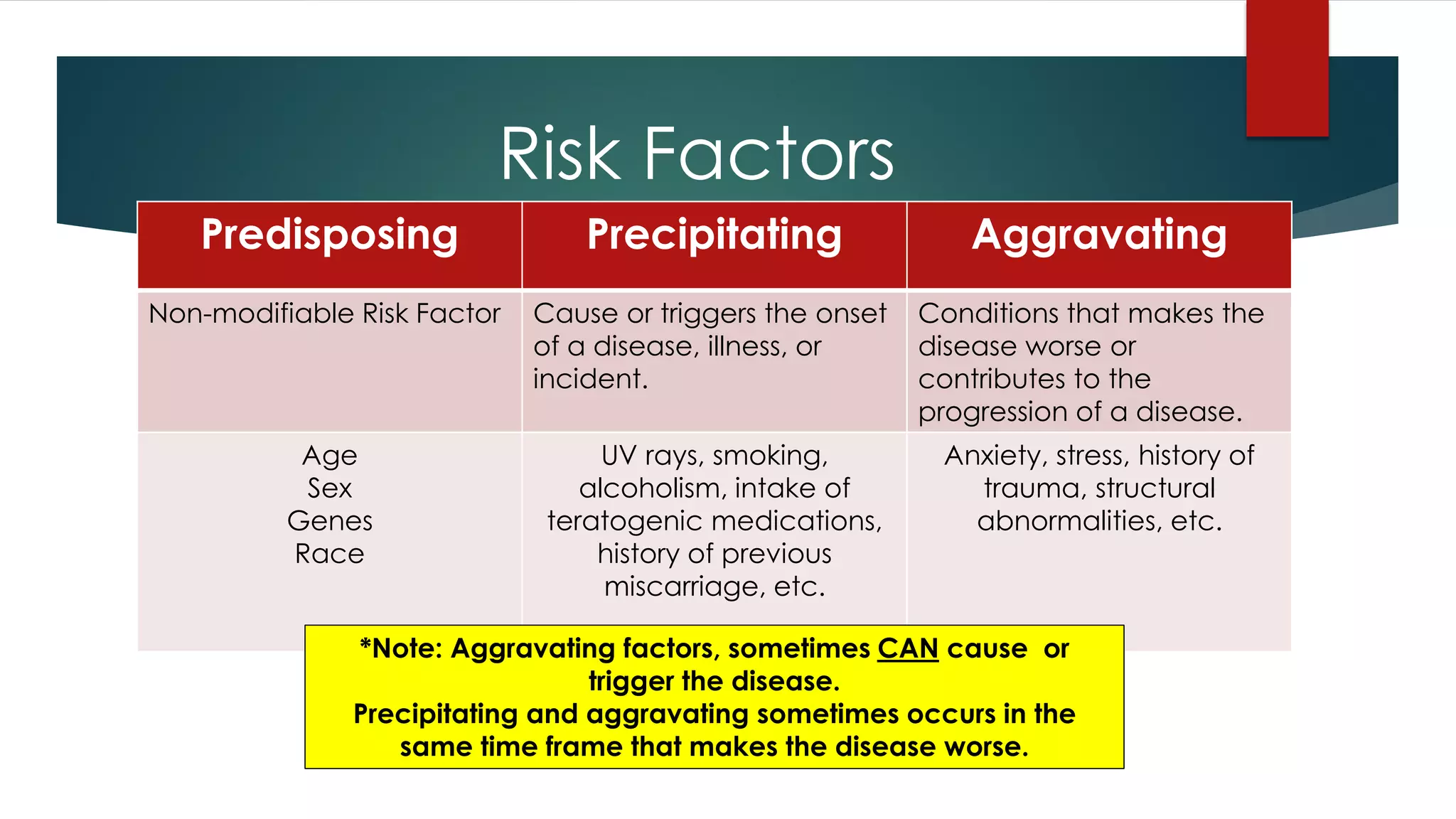
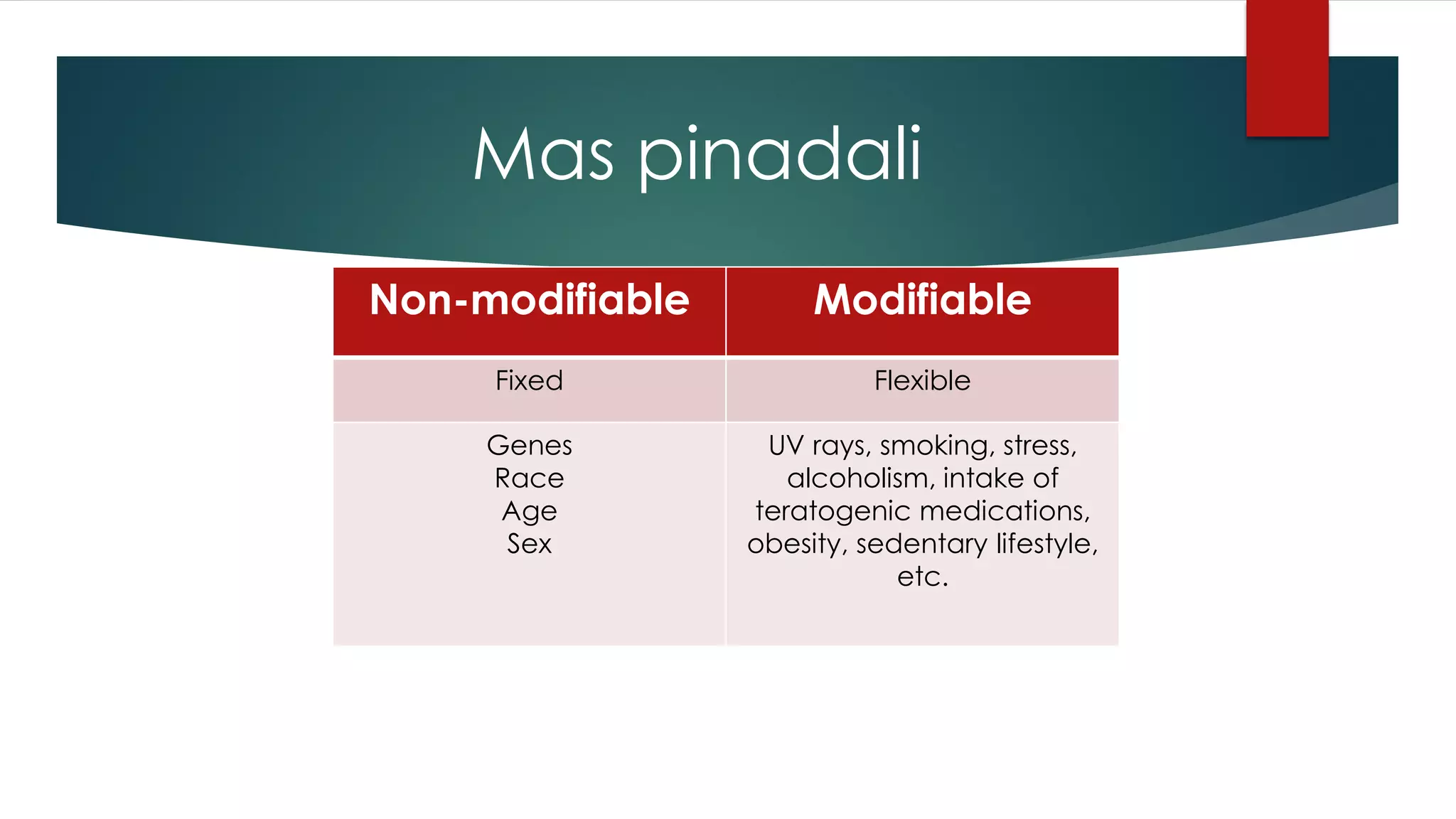
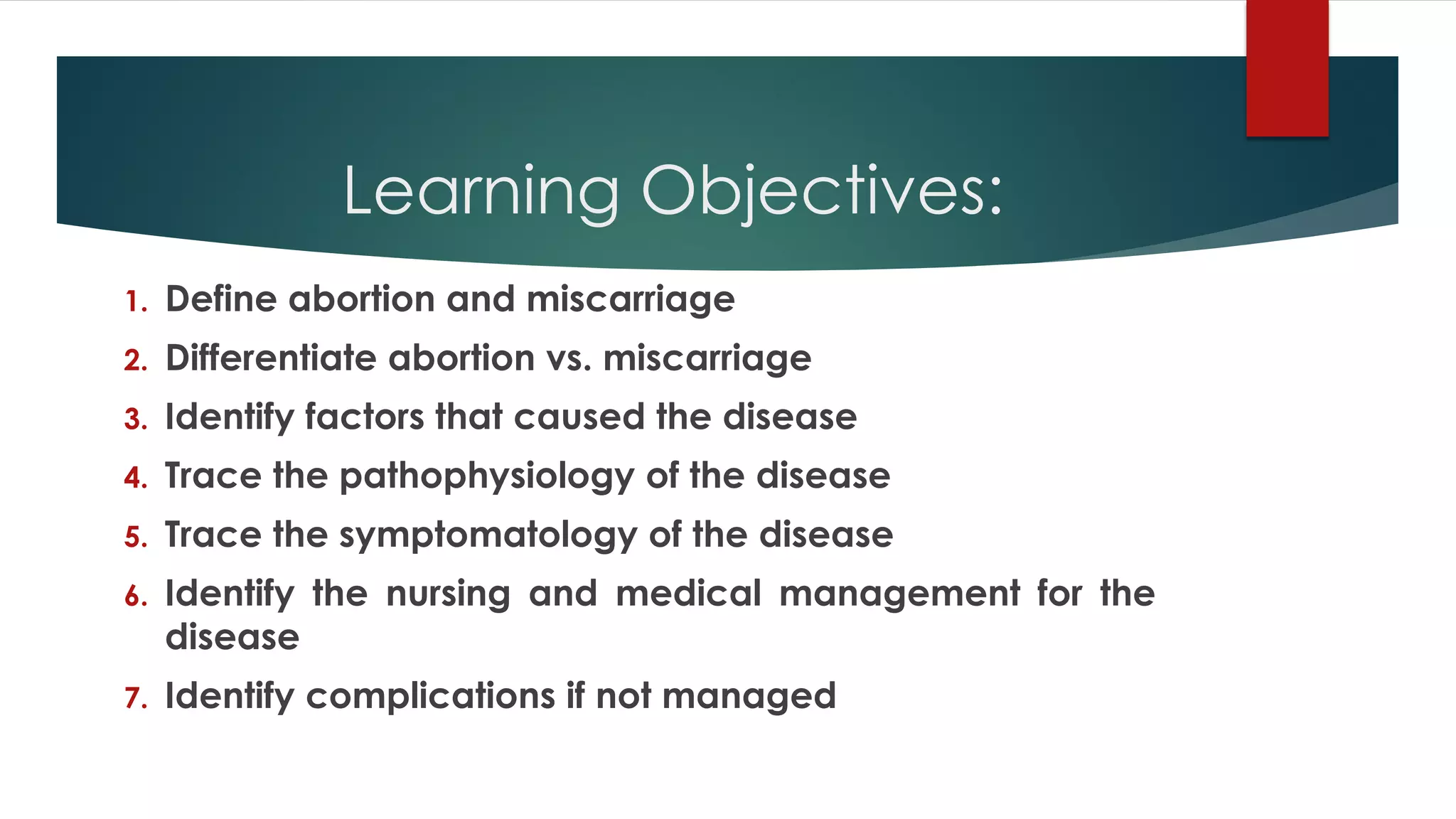
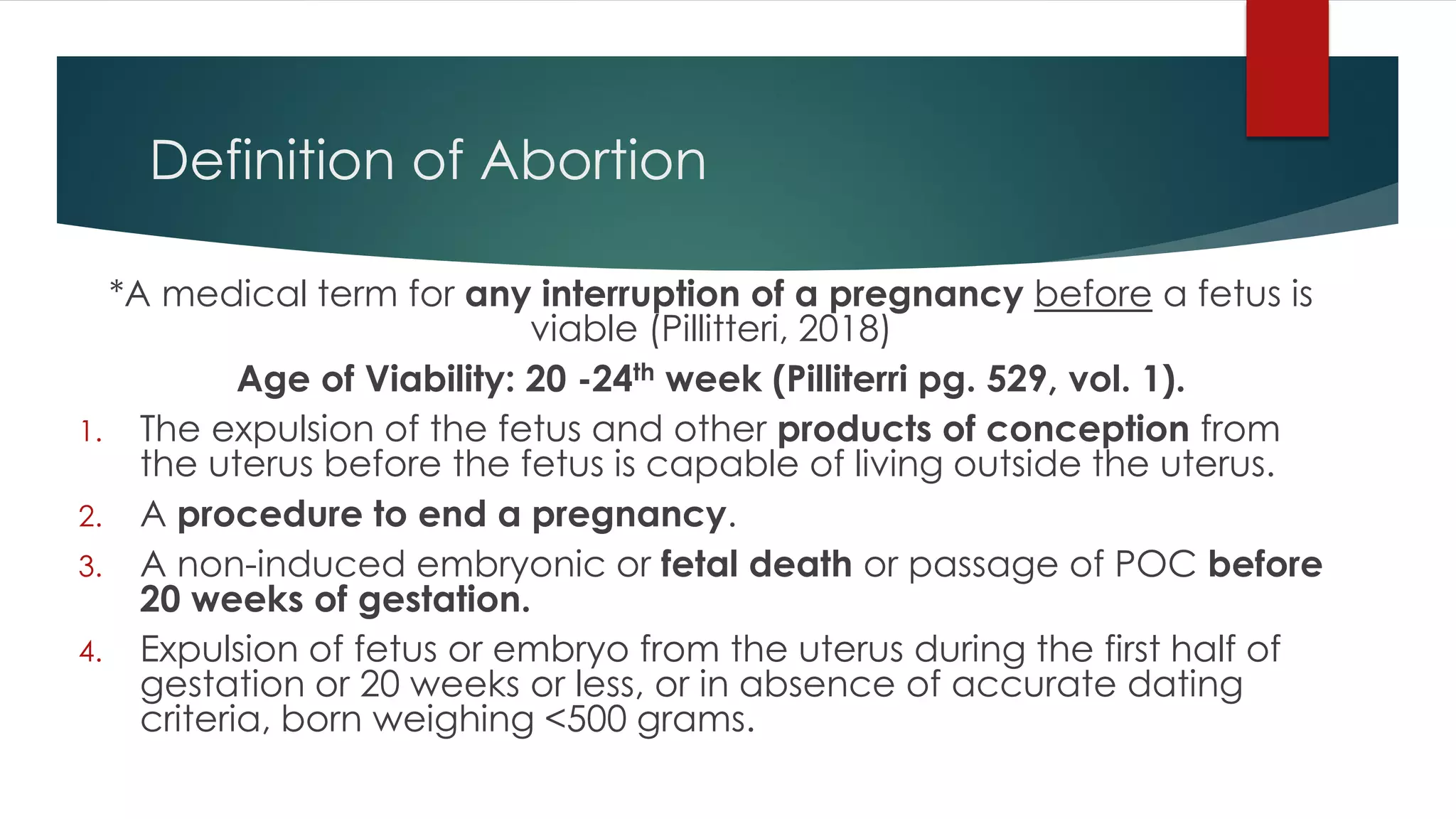
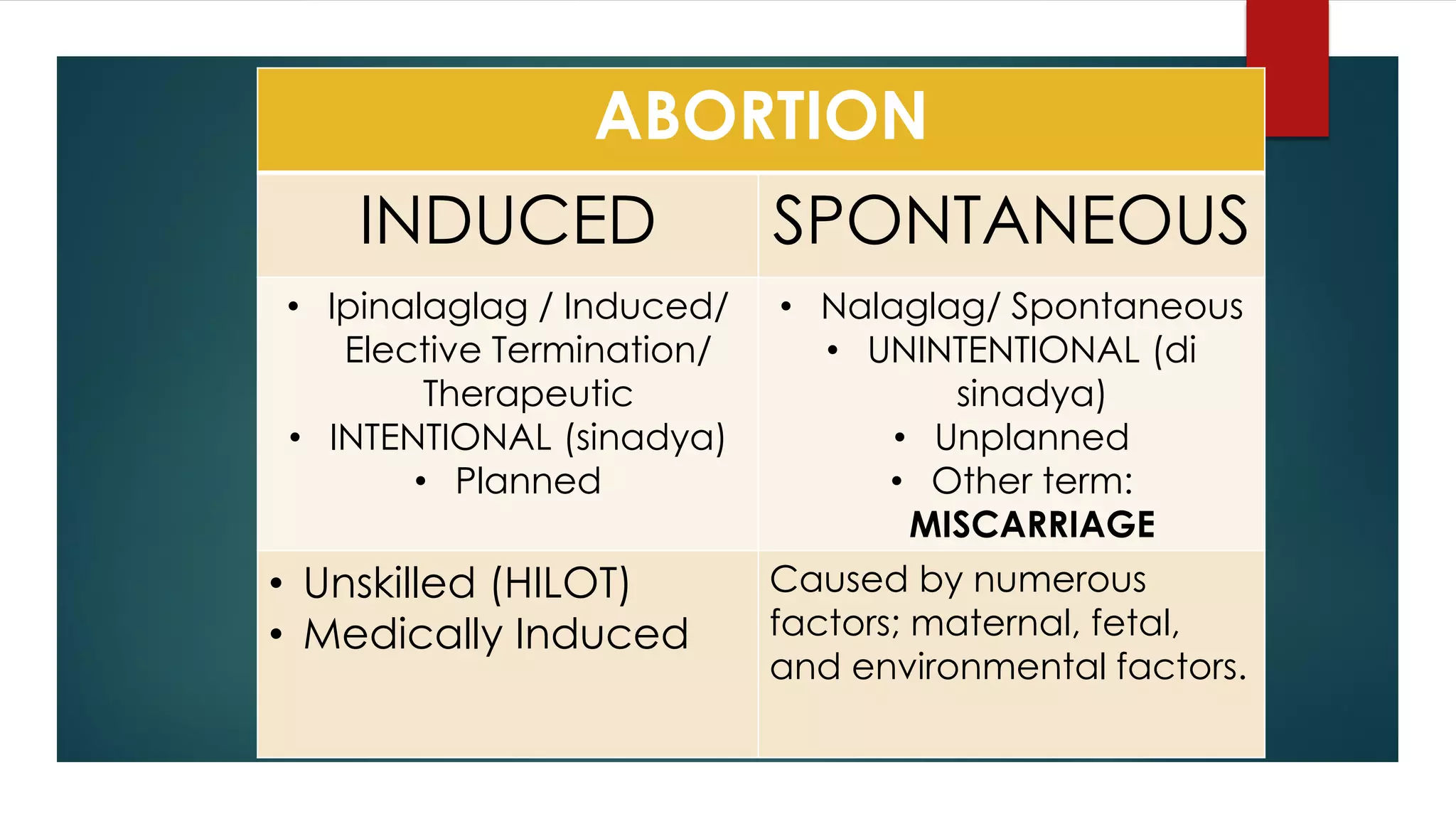
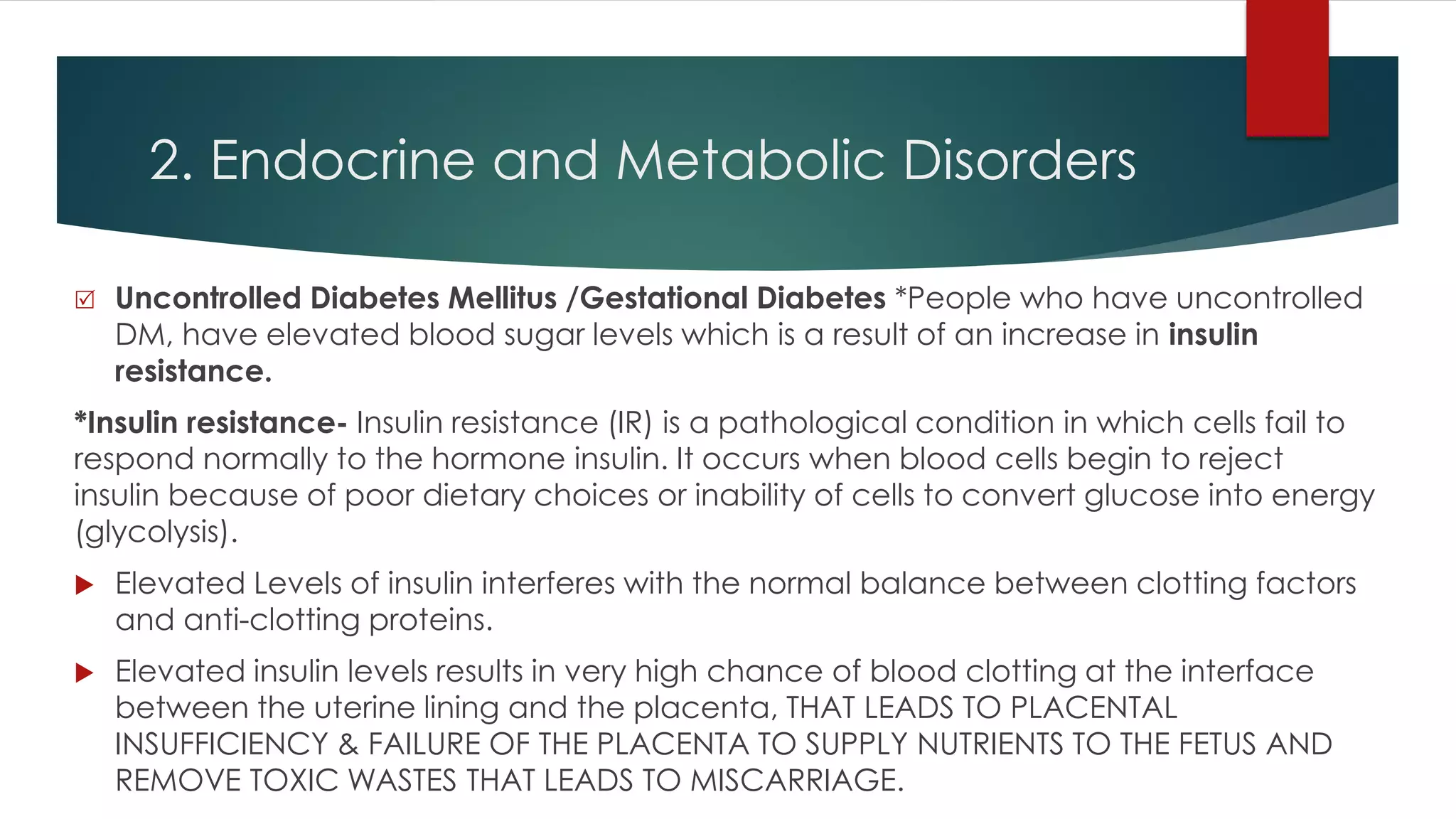
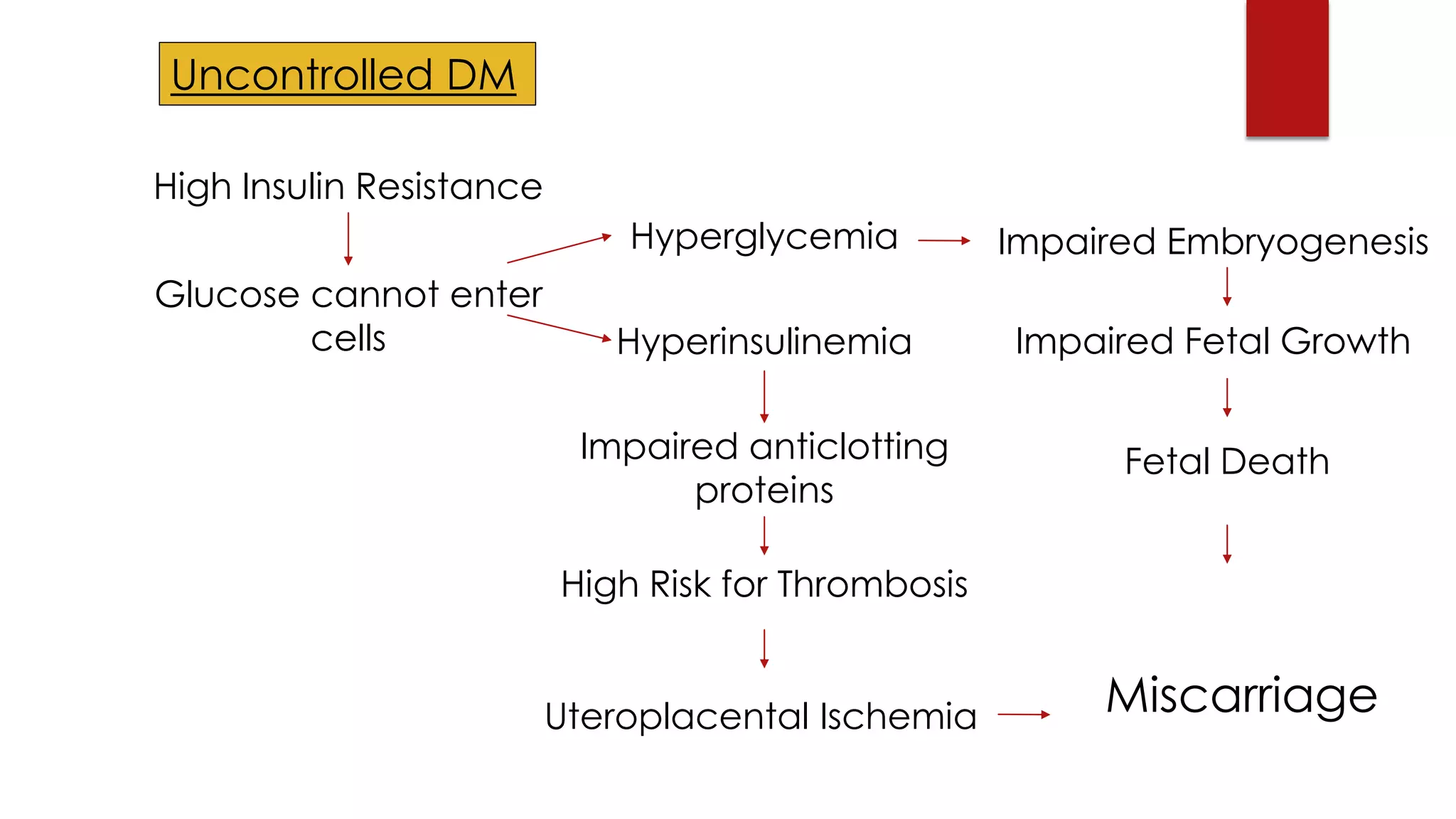
This document provides an introduction to pathophysiology. It begins by defining pathophysiology as the functional changes associated with or resulting from disease or injury, and the study of changes in the way the body works due to disease. The document then discusses several topics related to pathophysiology including normal vs abnormal body functions, clinical manifestations of disease, risk factors, and provides examples of pathophysiological processes and clinical manifestations for diabetes mellitus.