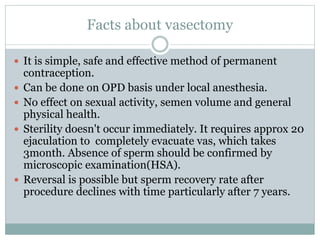
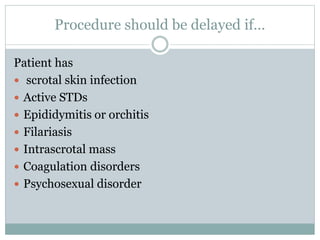
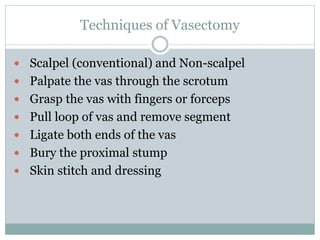
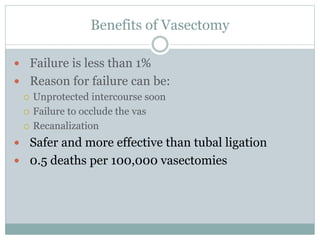
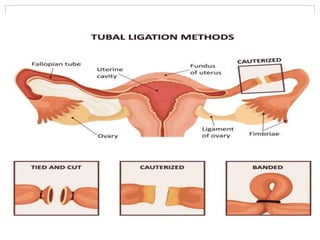
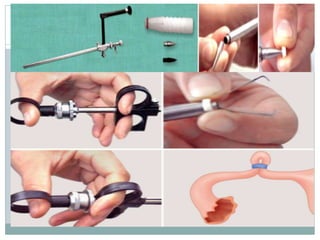
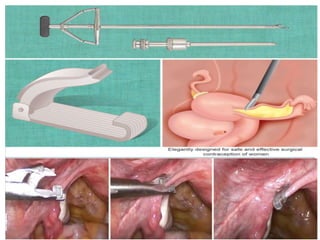
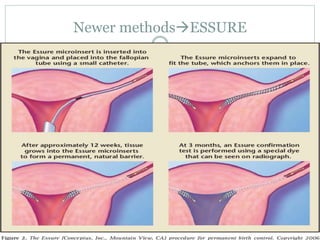
This document discusses permanent contraception options for men and women, including vasectomies and tubal ligations. It provides details on the procedures, such as vasectomies involving transecting and occluding the vas deferens through non-scalpel or scalpel methods. Tubal ligations can be performed through abdominal, laparoscopic, or vaginal approaches. Both procedures are generally safe and effective but require extensive counseling as they provide permanent sterilization.