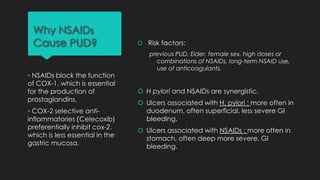
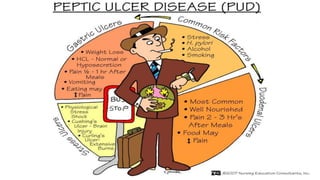
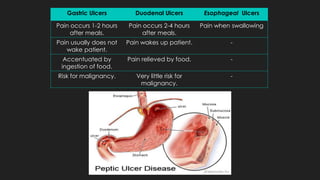
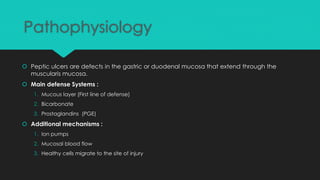
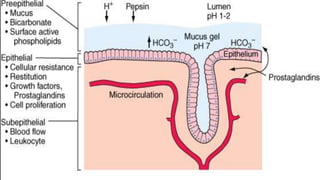
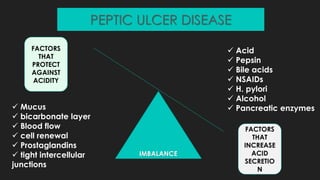
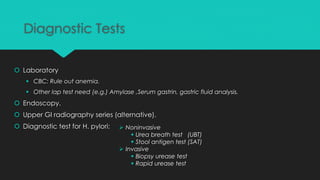
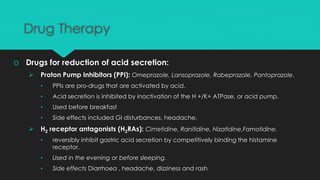
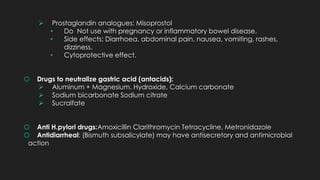
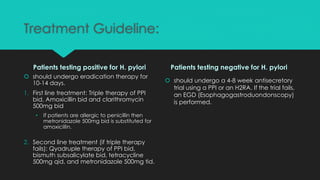
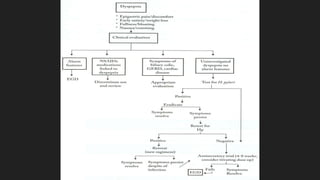
Peptic ulcer disease is characterized by sores in the stomach, duodenum, or esophagus caused by an imbalance between gastric acid and mucosal defenses. Common causes include H. pylori infection, NSAIDs, smoking, alcohol, and stress. Symptoms may include dyspepsia, abdominal pain, nausea, and weight loss. Complications can include gastrointestinal bleeding, perforation, and cancer. Diagnosis involves endoscopy and tests for H. pylori. Treatment focuses on reducing acid with PPIs or H2 blockers, eradicating H. pylori with antibiotic therapy, and lifestyle modifications.