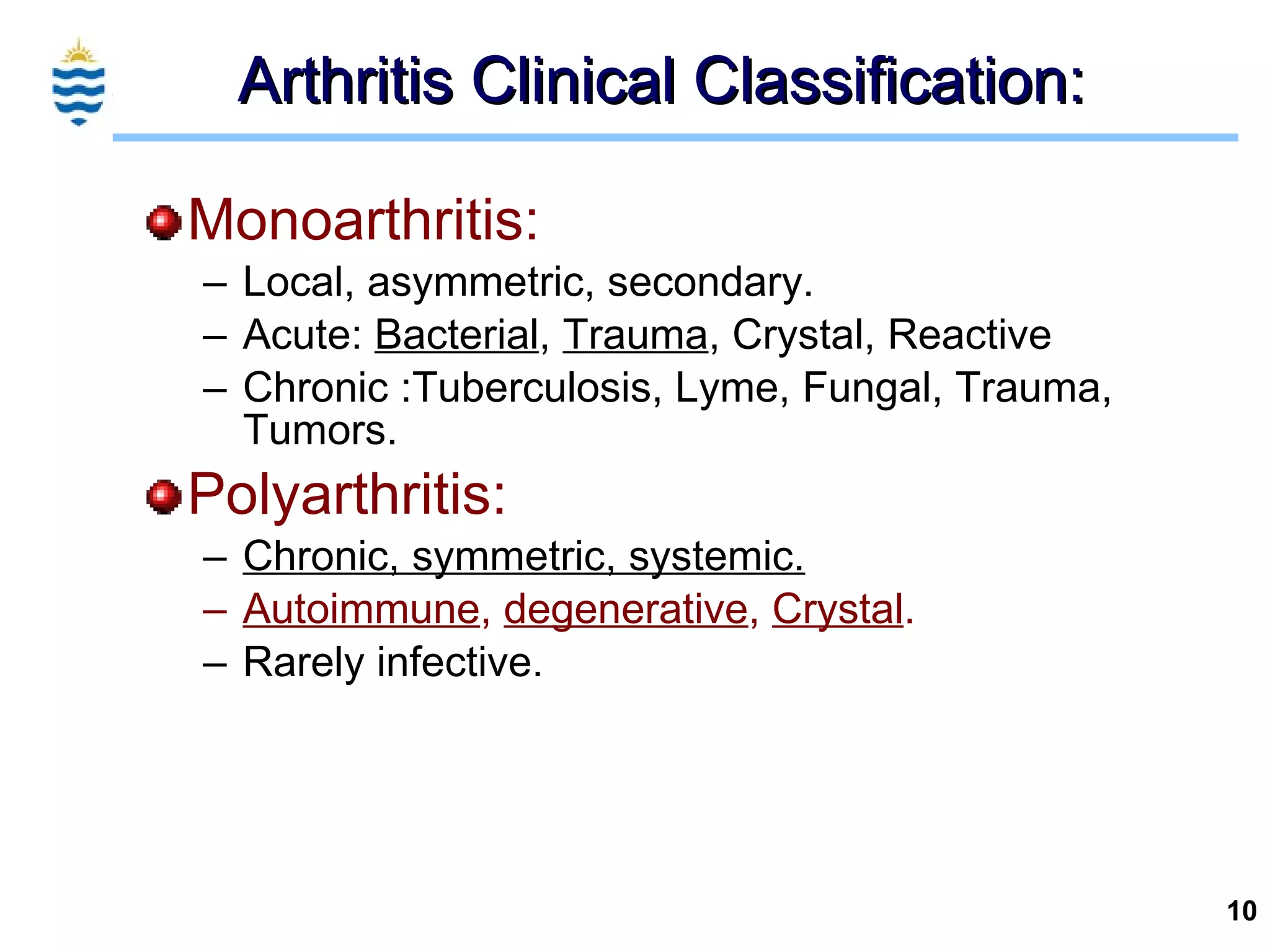
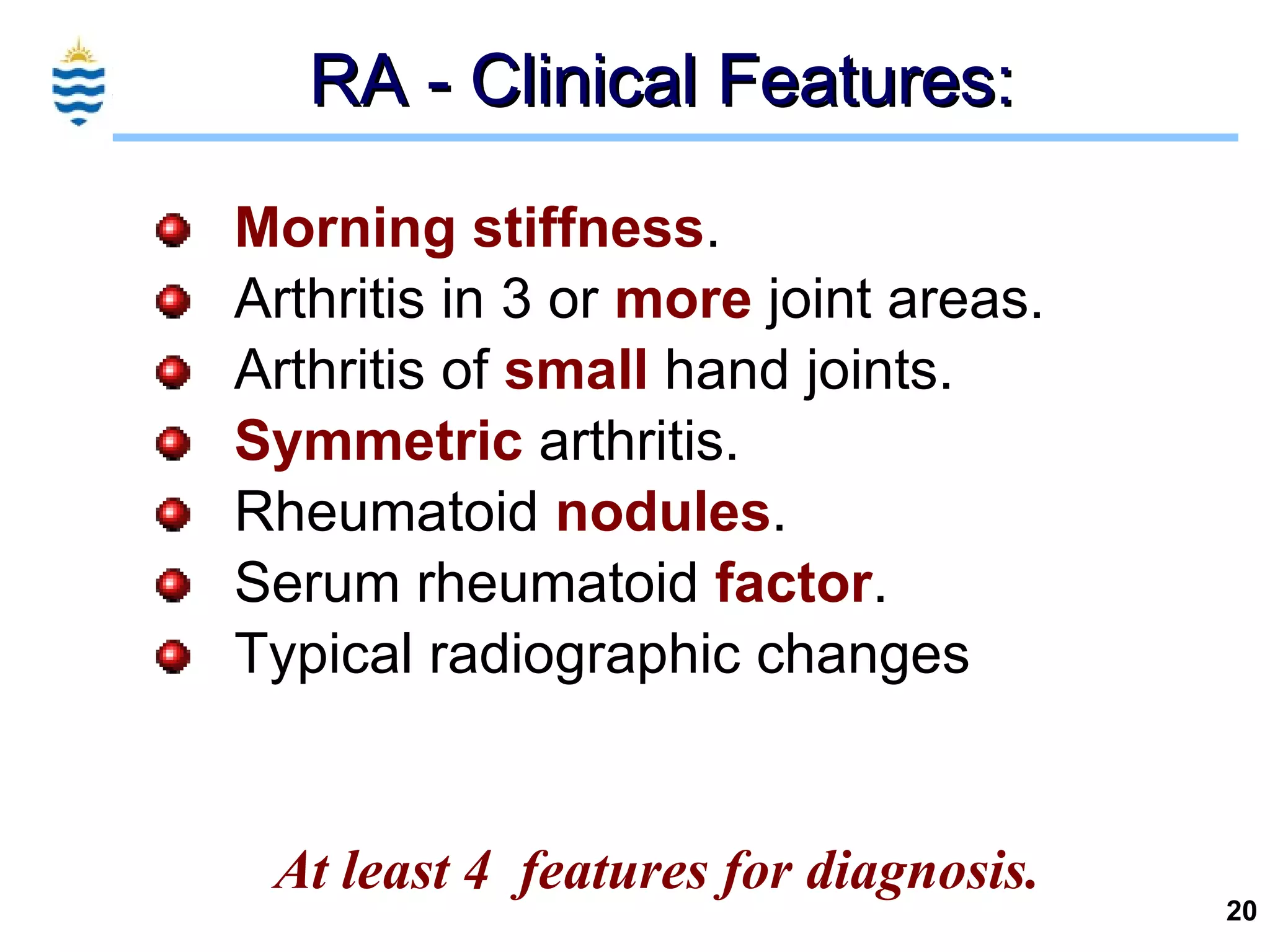
This document discusses various types of arthritis, including their signs, symptoms, pathogenesis, and clinical features. Rheumatoid arthritis is an autoimmune disease that causes proliferative synovitis and often progresses to joint destruction. Osteoarthritis is a degenerative joint disease that causes cartilage erosion and bone changes like osteophyte formation. Gout is caused by deposition of urate crystals in the joints. Other arthritides discussed include psoriatic arthritis, septic arthritis, and calcium pyrophosphate deposition disease.