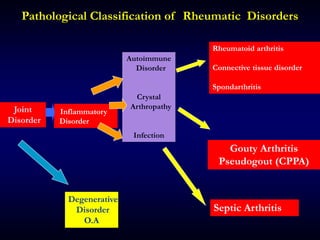
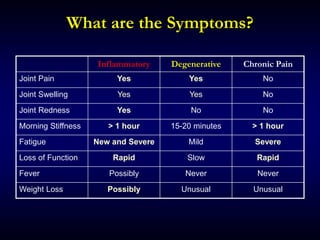
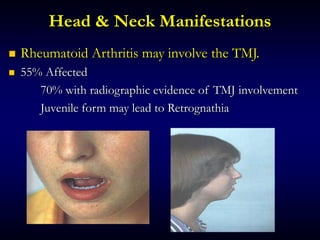
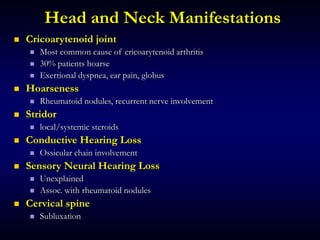
This document provides an overview of various rheumatologic disorders including their classification, symptoms, physical exam findings, and management considerations for dental patients. Key points include:
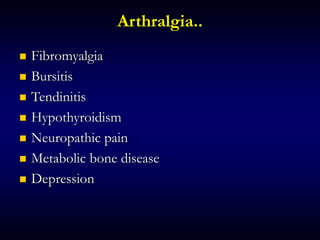
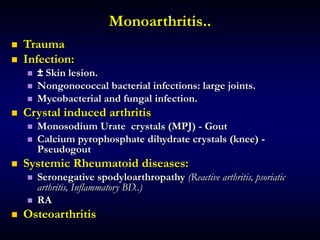
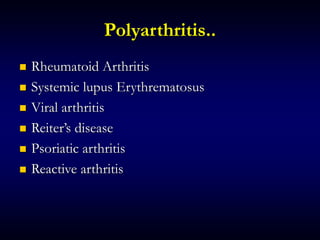
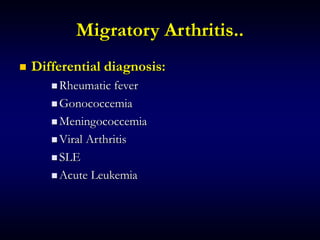
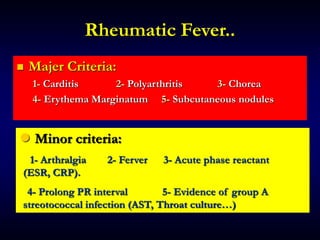
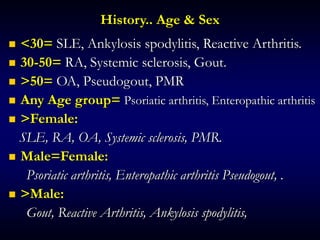
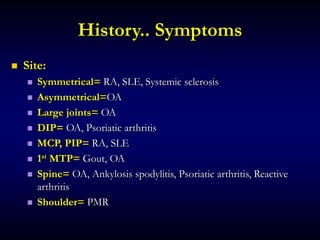
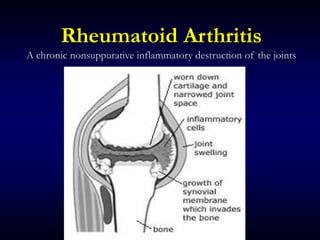
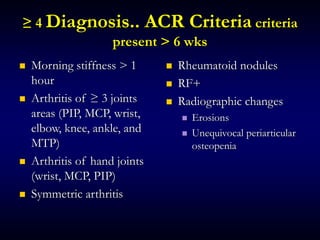
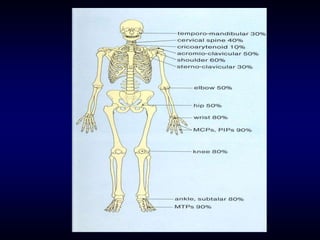
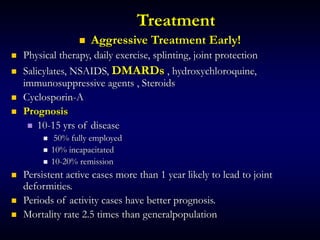
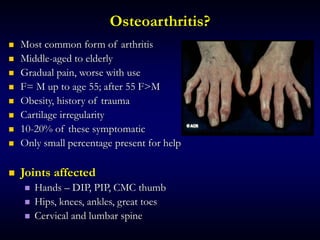
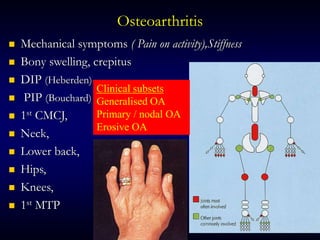
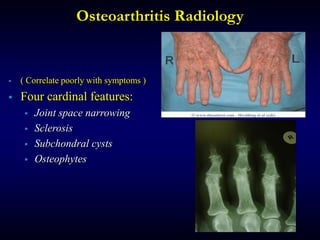
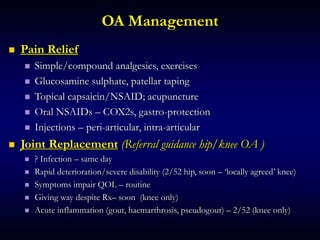
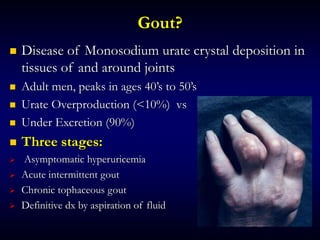
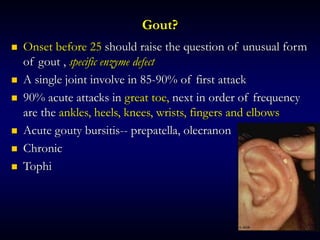
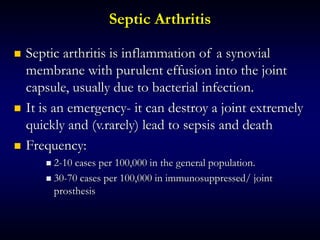
1. Rheumatologic disorders are classified as joint, degenerative, inflammatory, connective tissue, spondarthritis, autoimmune, or crystal arthropathy diseases. Common conditions discussed are osteoarthritis, rheumatoid arthritis, and gout.
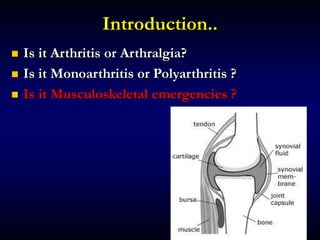
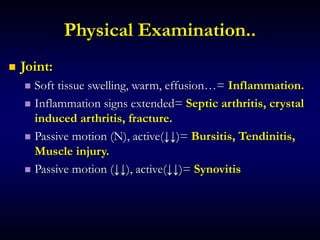
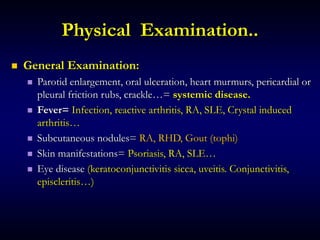
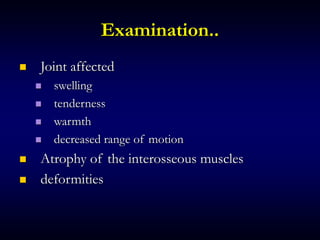
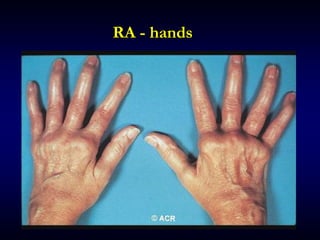
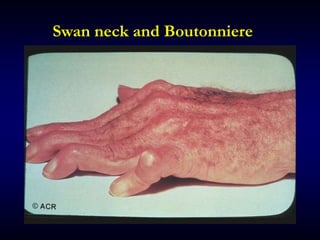
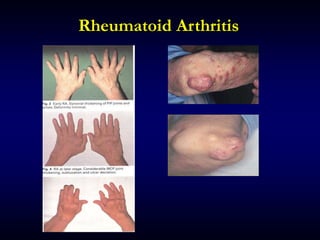
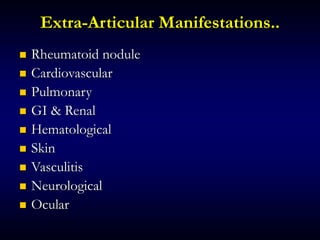
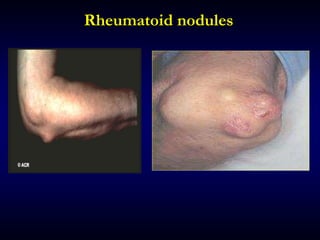
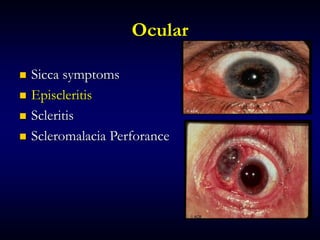
2. Physical exam findings help differentiate conditions based on factors like joint involvement, inflammation signs, range of motion, and presence of extra-articular manifestations.
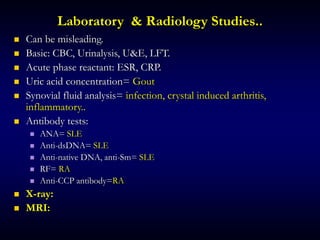
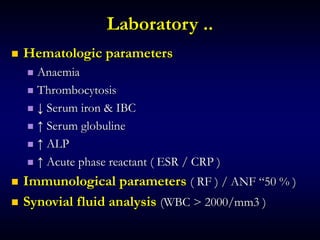
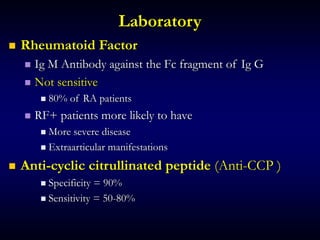
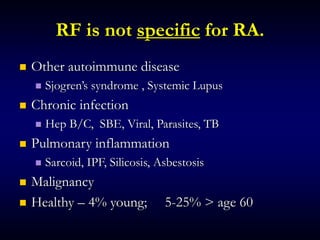
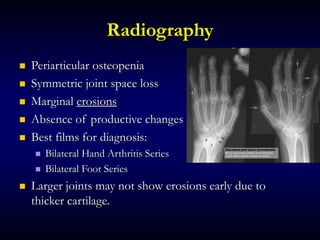
3. Laboratory/radiology tests are used to confirm diagnoses but can be misleading. Synovial fluid analysis and antibody/acute phase reactant testing