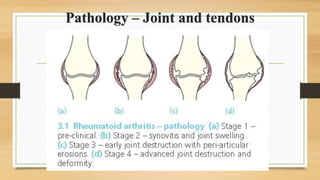
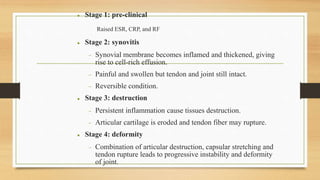
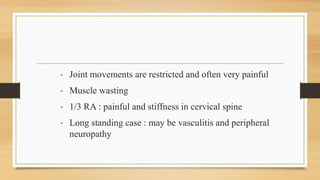
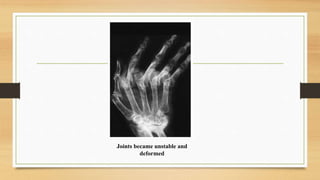
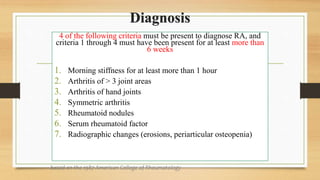
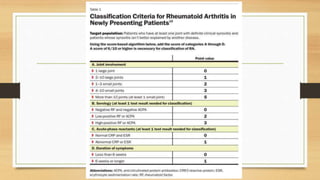
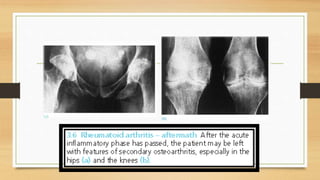
Rheumatoid arthritis is a chronic autoimmune disease that causes inflammation of the synovium and leads to joint damage over time. It is influenced by genetic, environmental, and hormonal factors. The inflammation causes swelling, stiffness, and pain in the joints. If left untreated, it can result in joint deformity and erosion of cartilage and bone. Treatment focuses on controlling inflammation, preventing deformity, and rehabilitation. Medications include NSAIDs, DMARDs, and biologics, along with physical therapy and surgery in some cases.