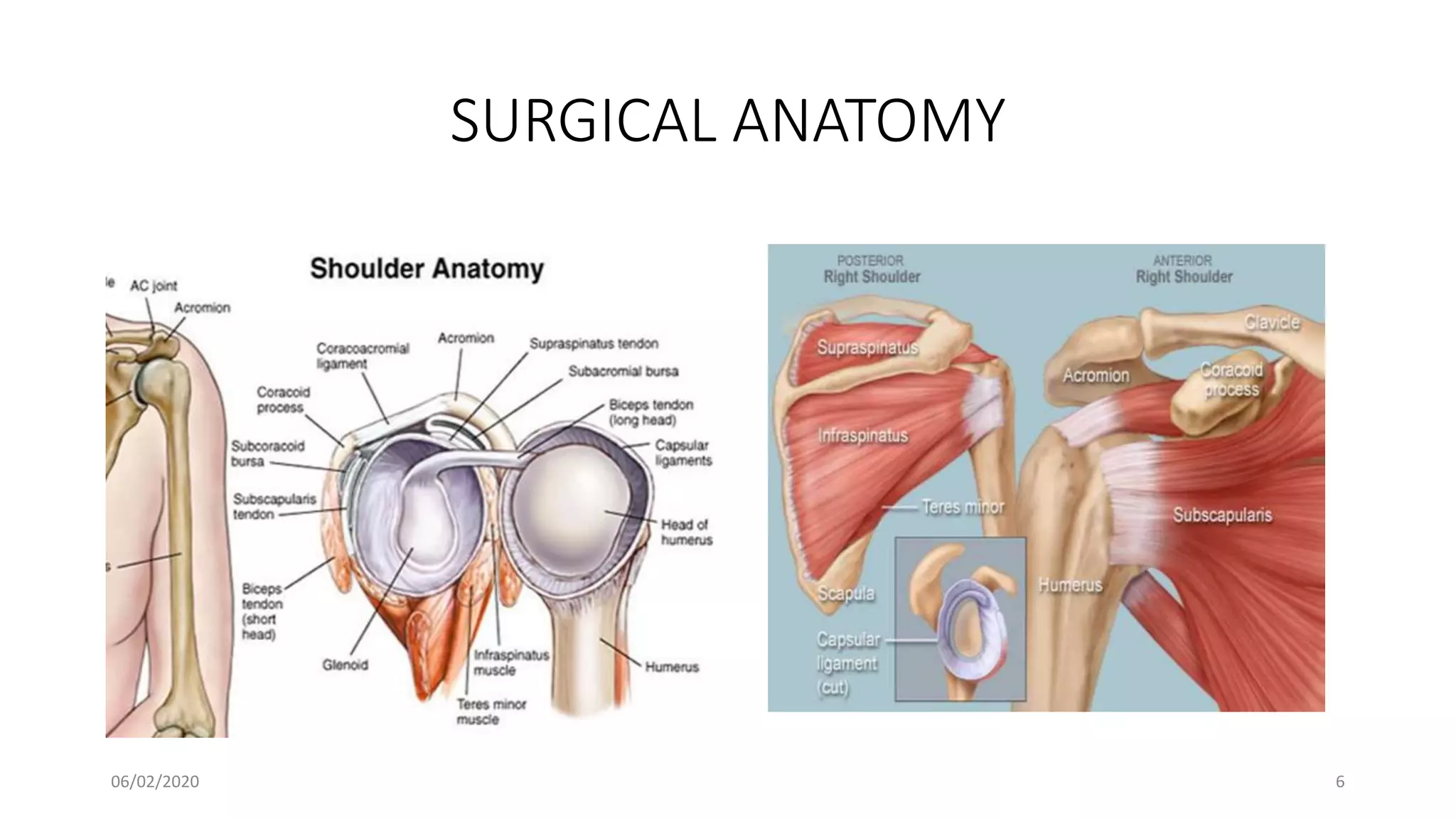
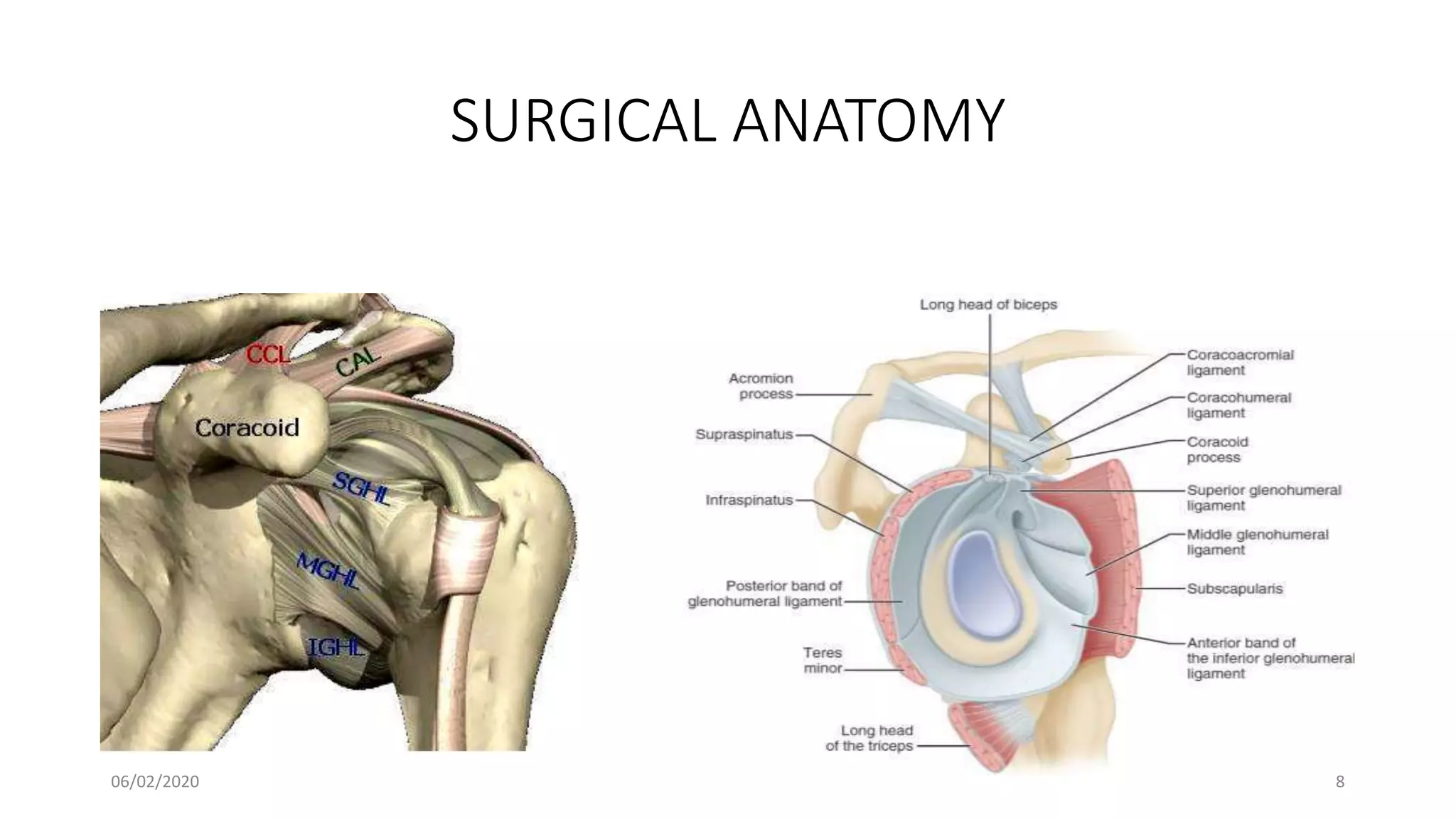
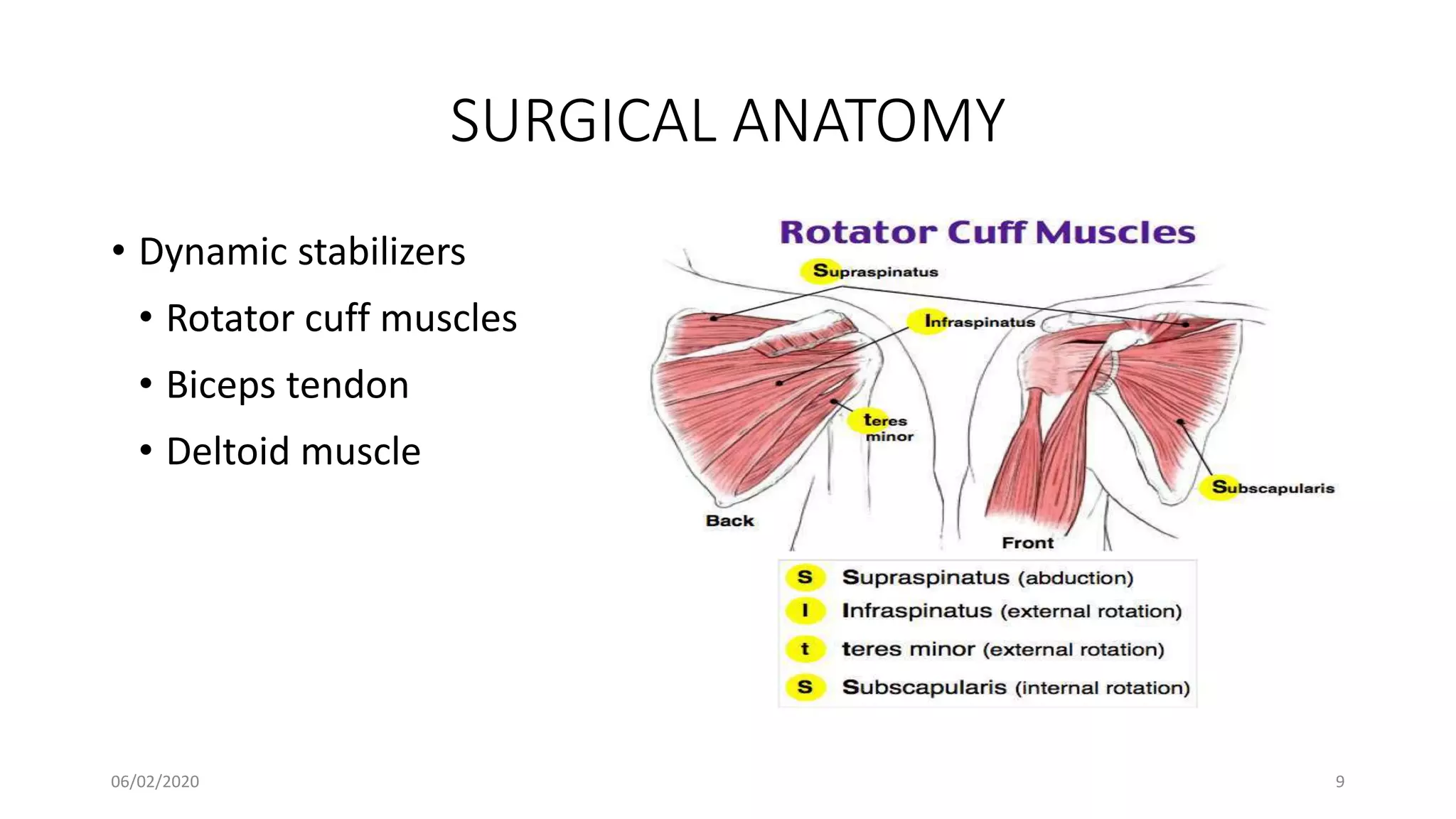
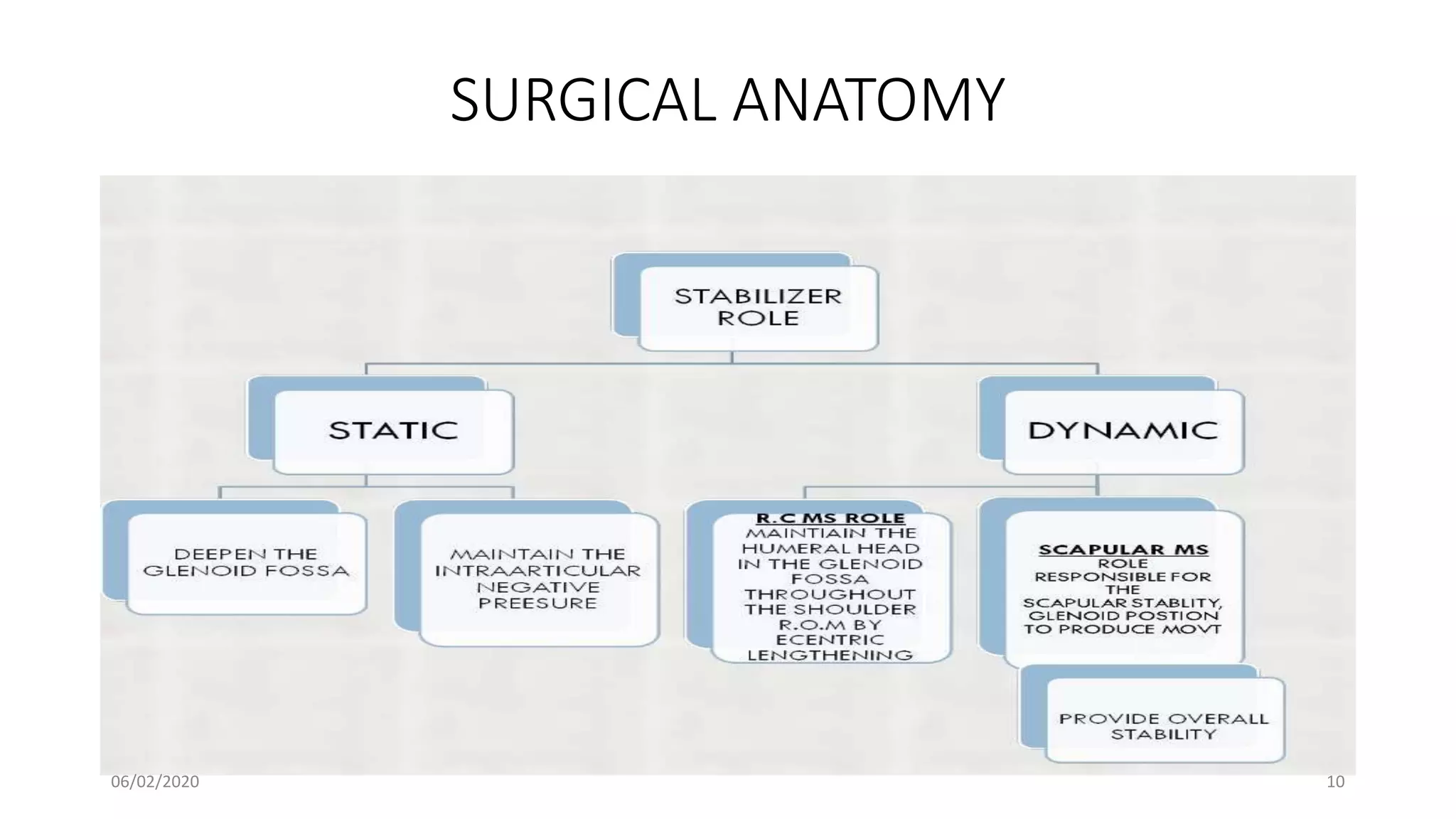
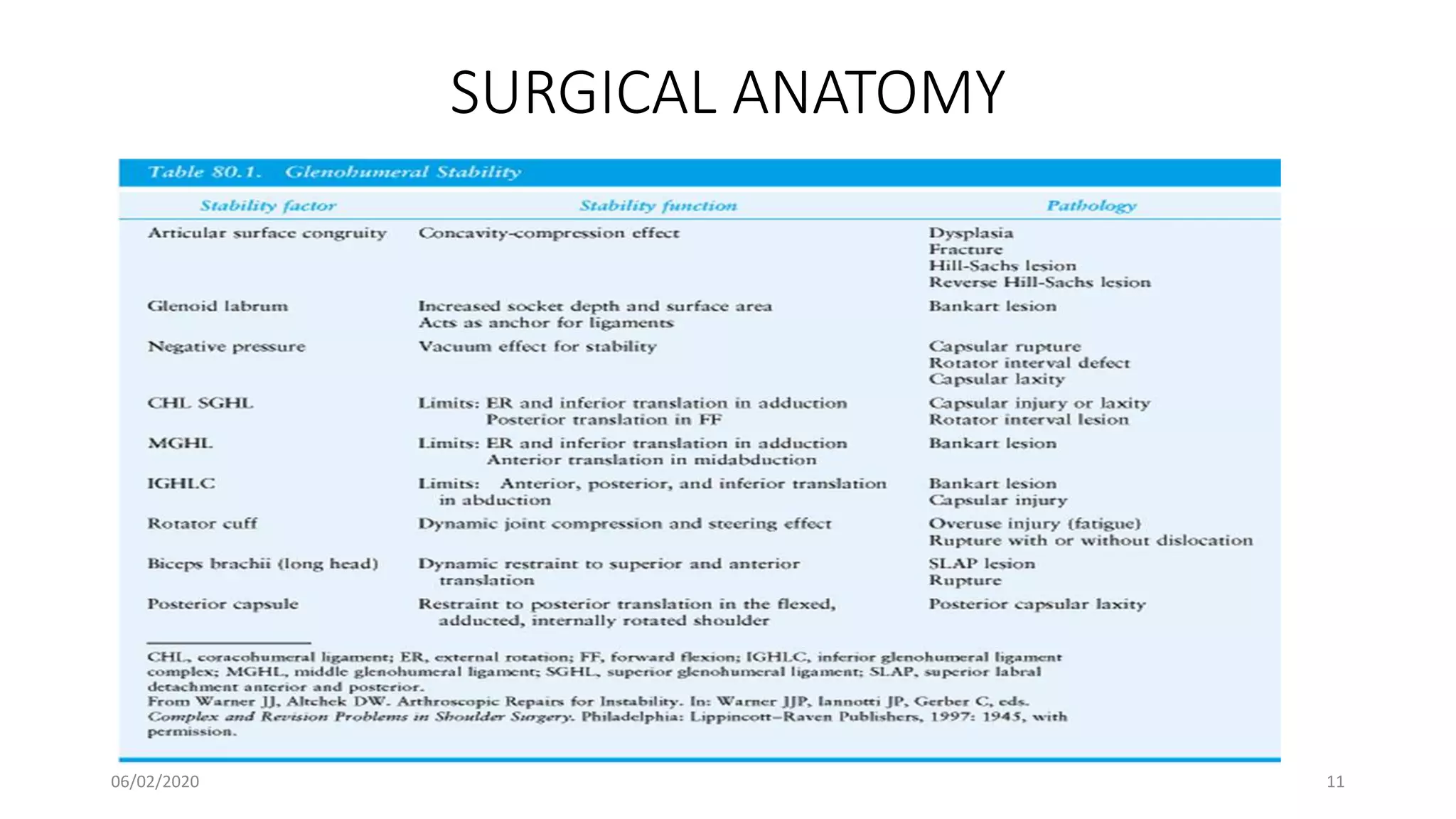
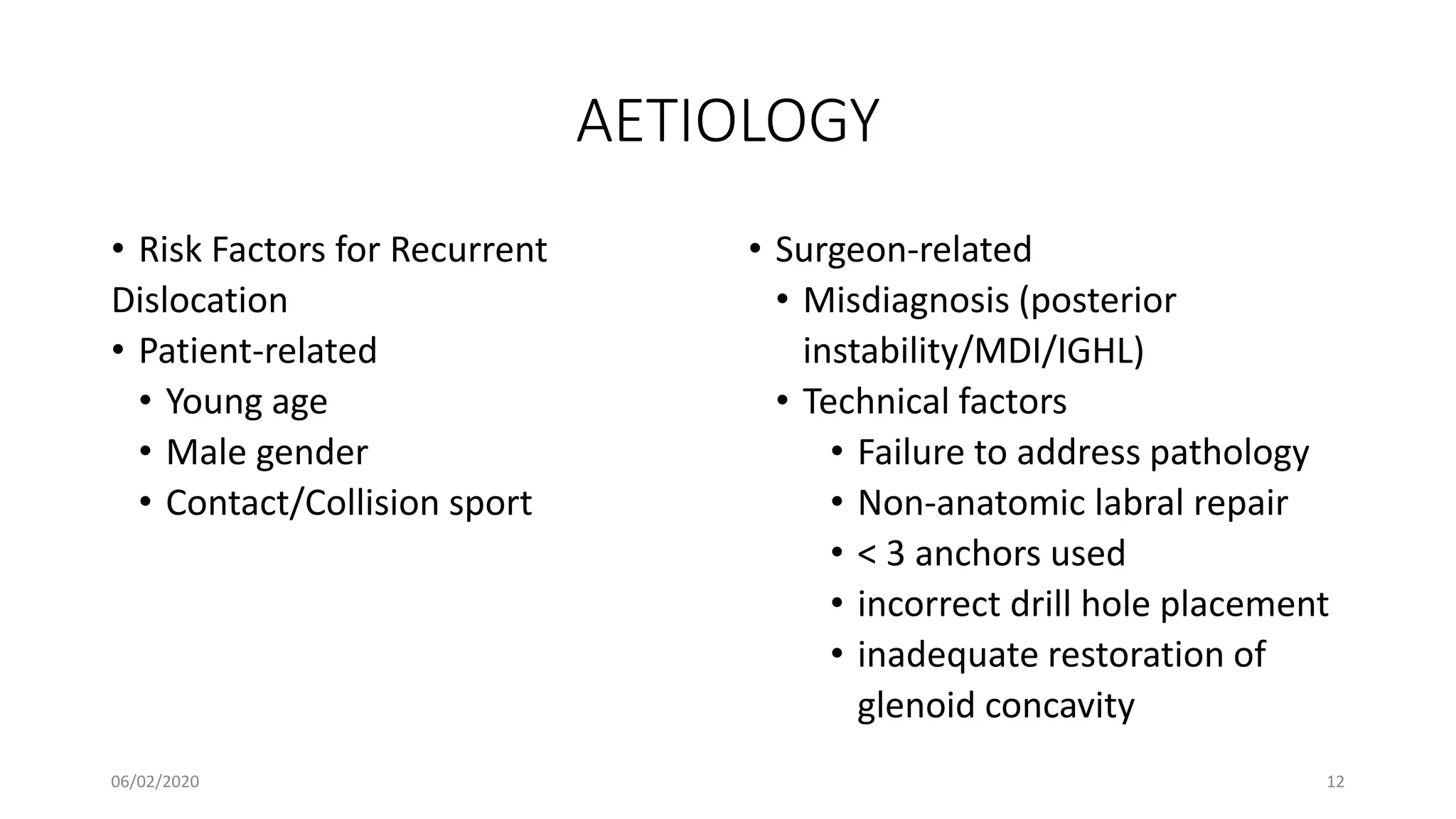
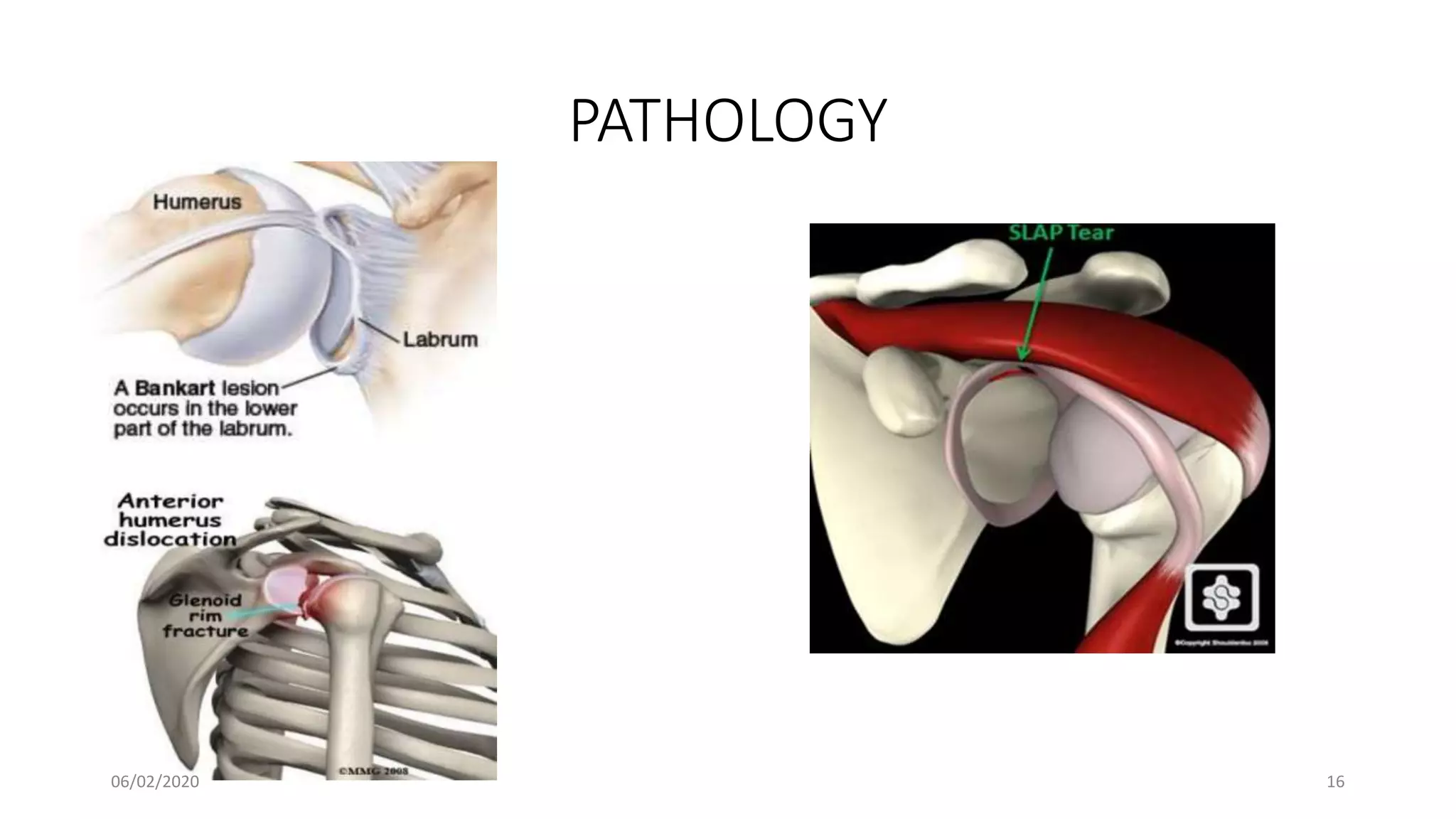
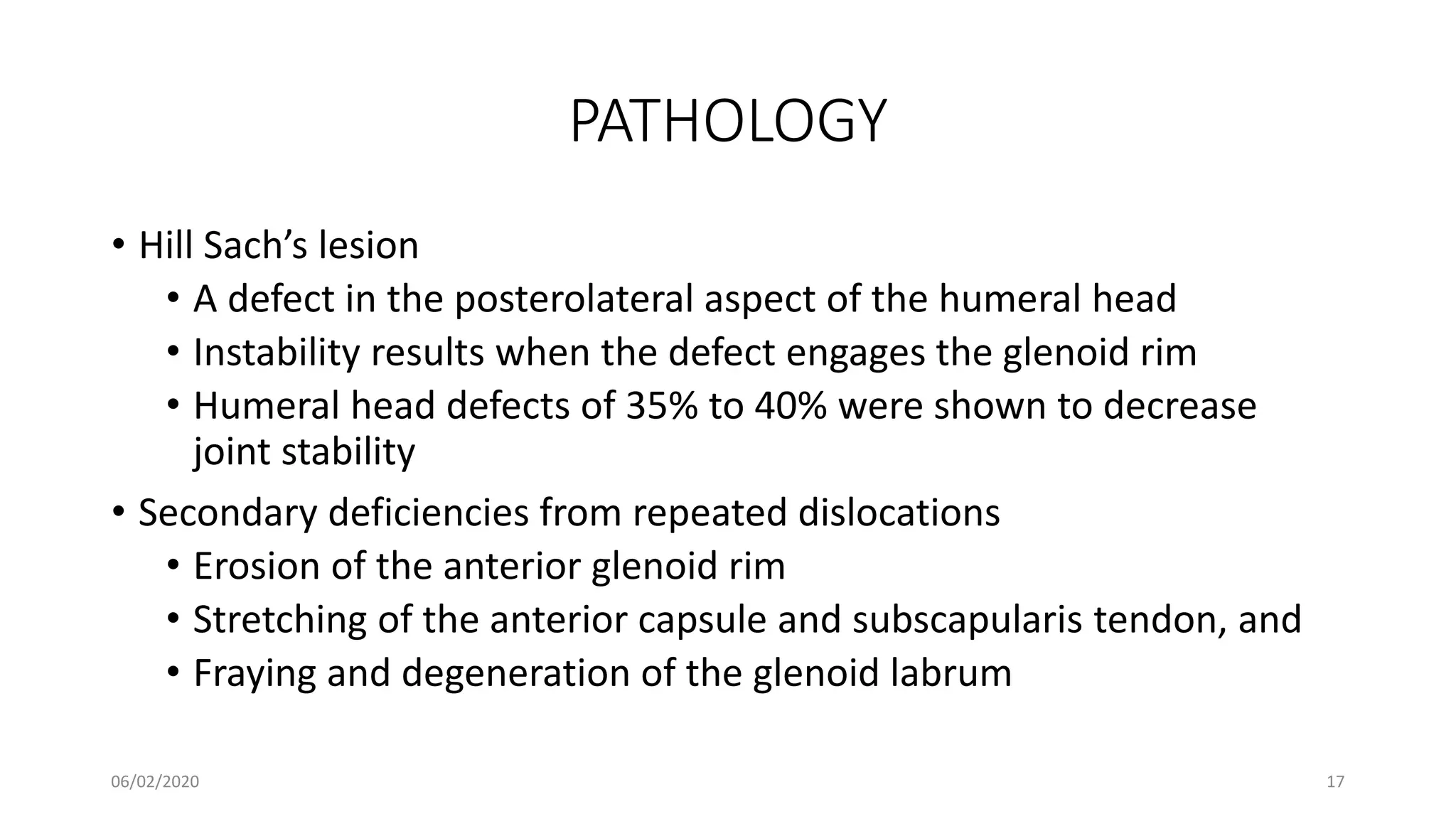
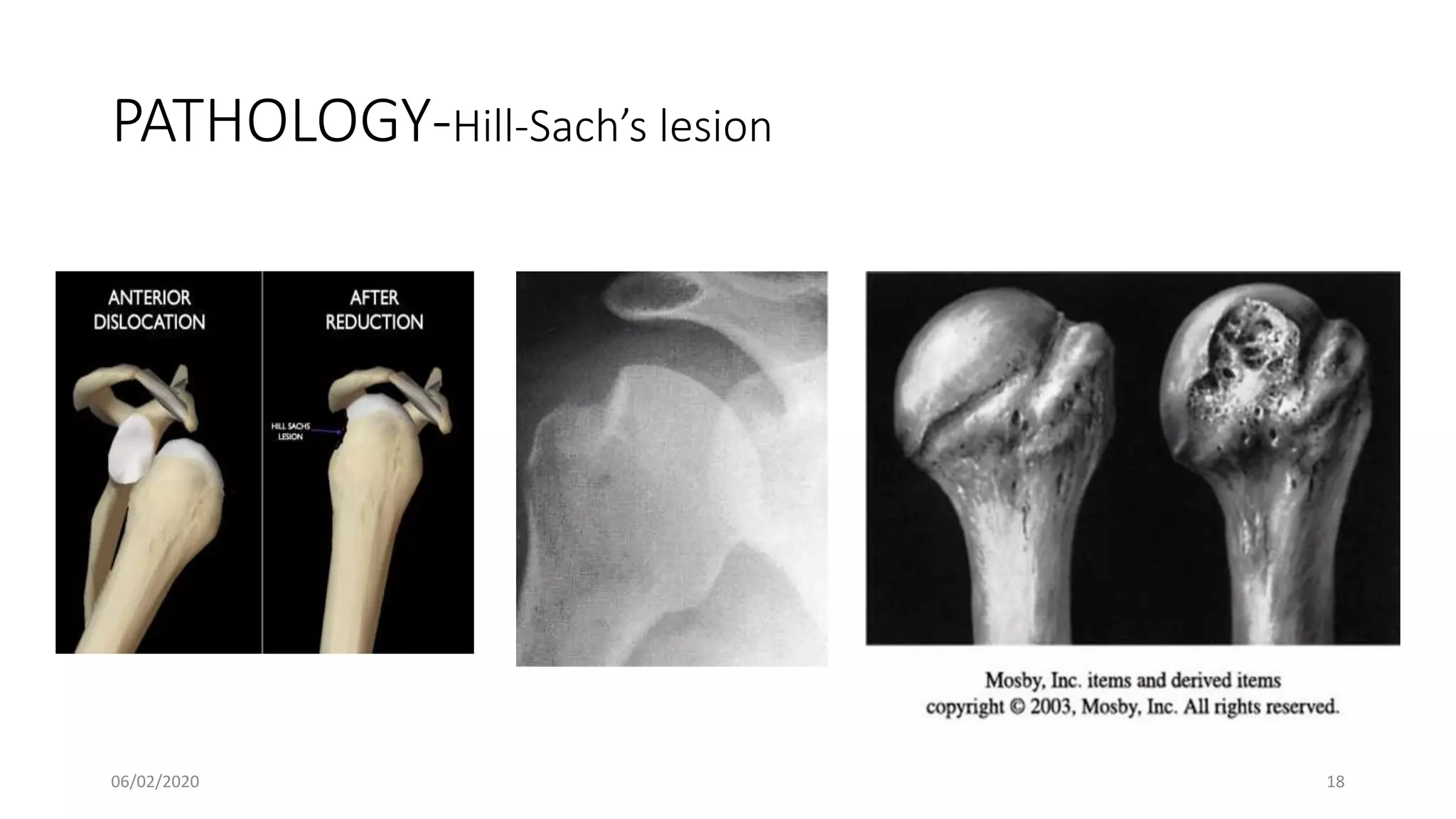
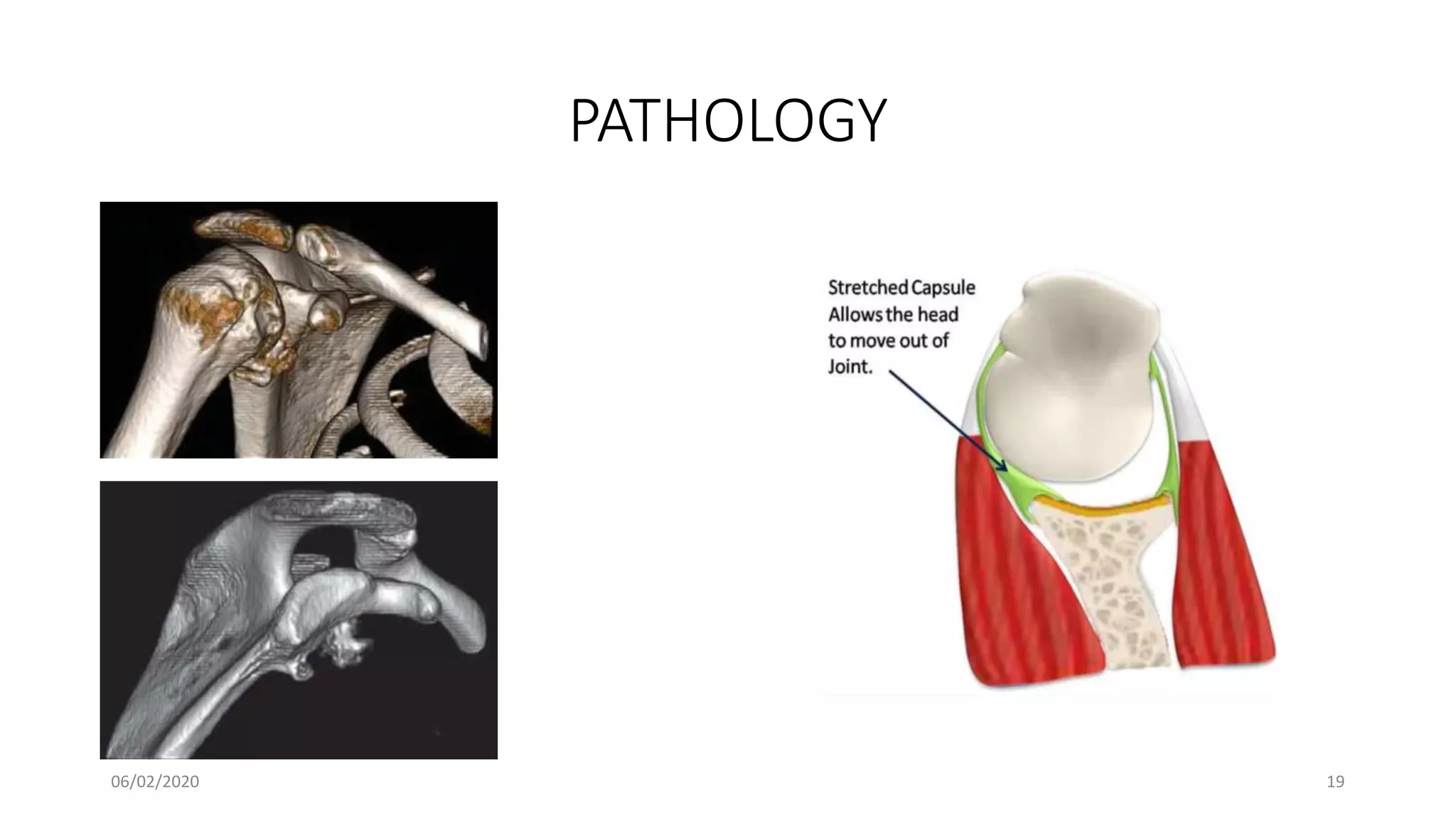
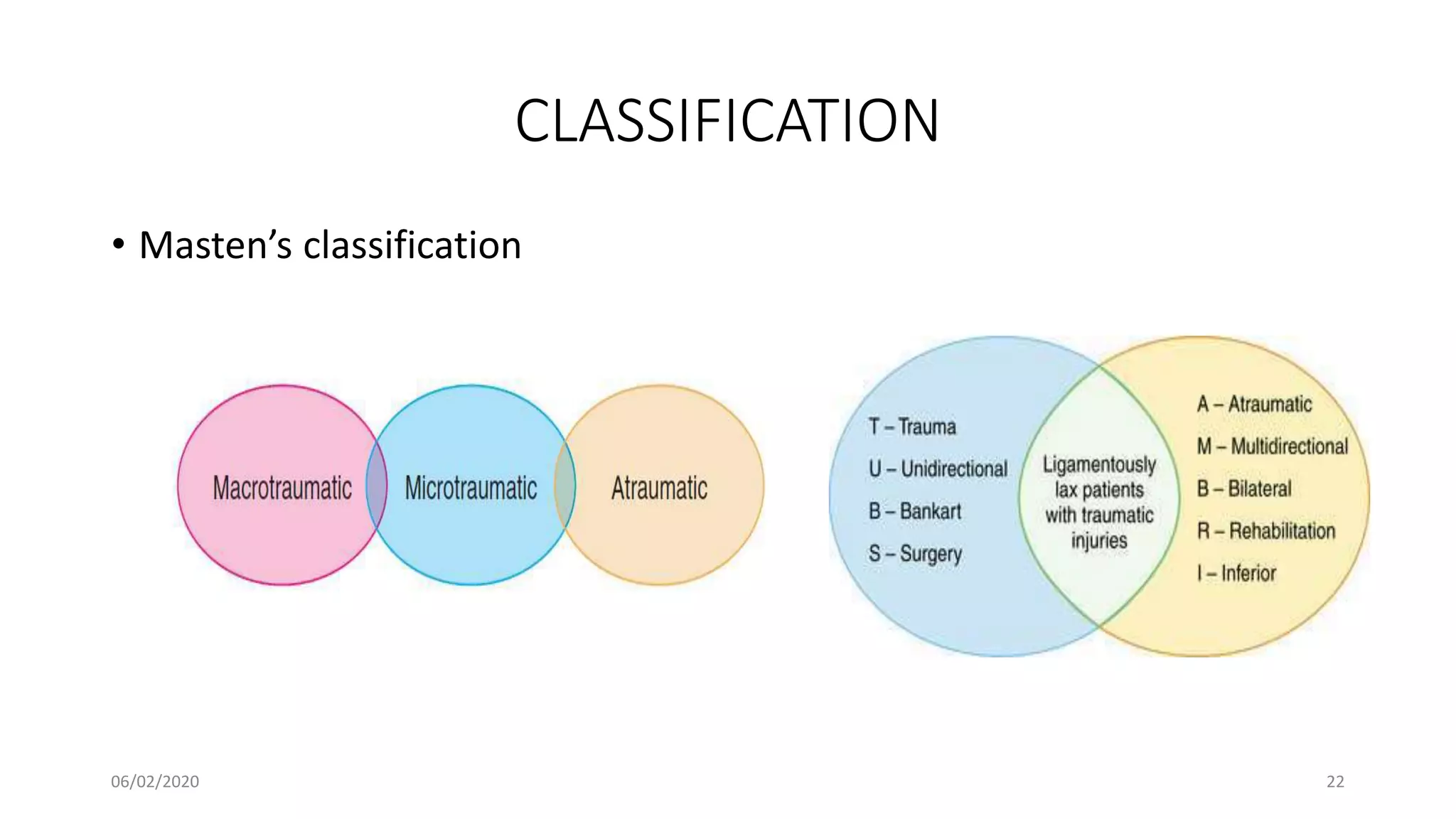
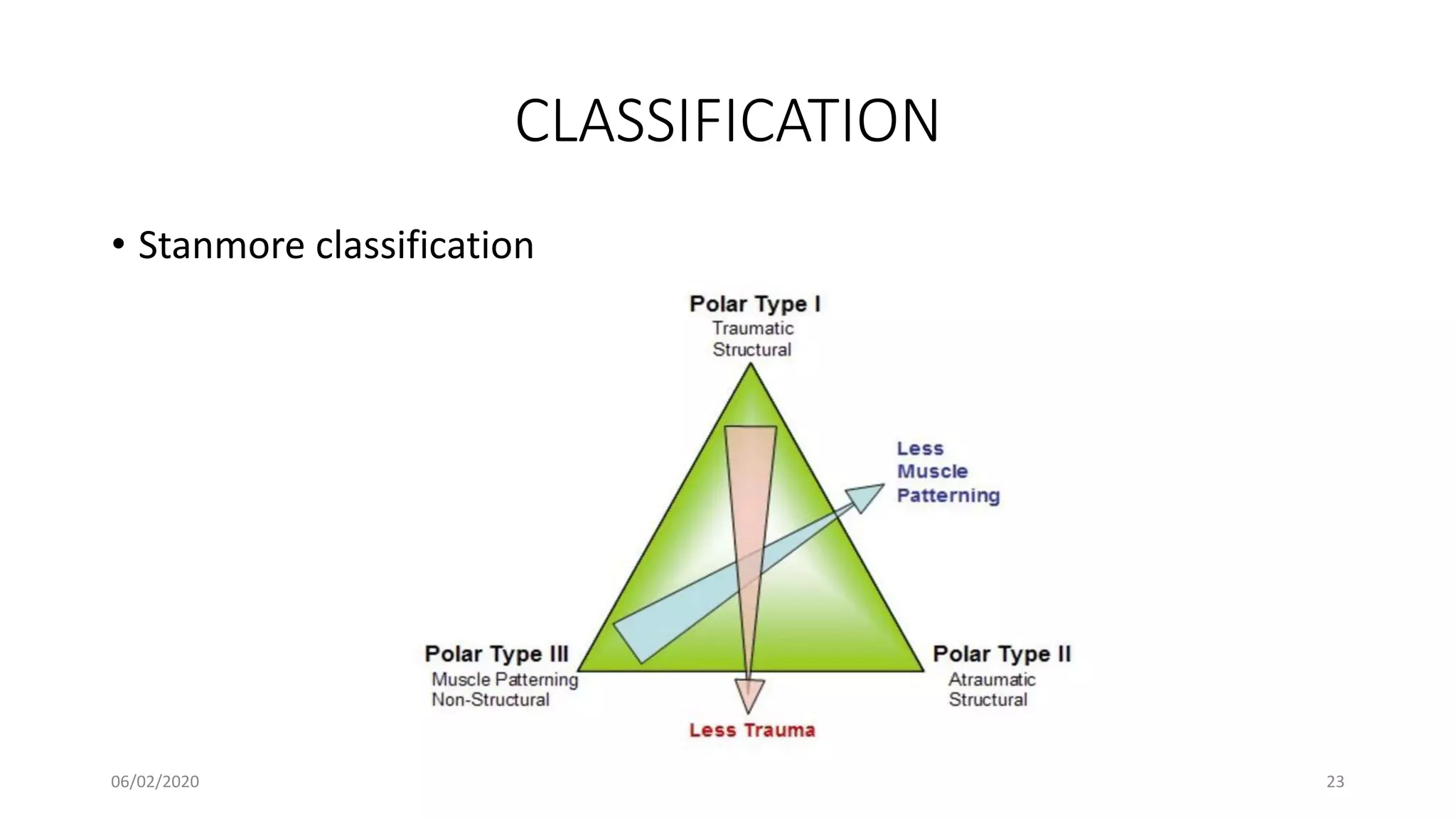
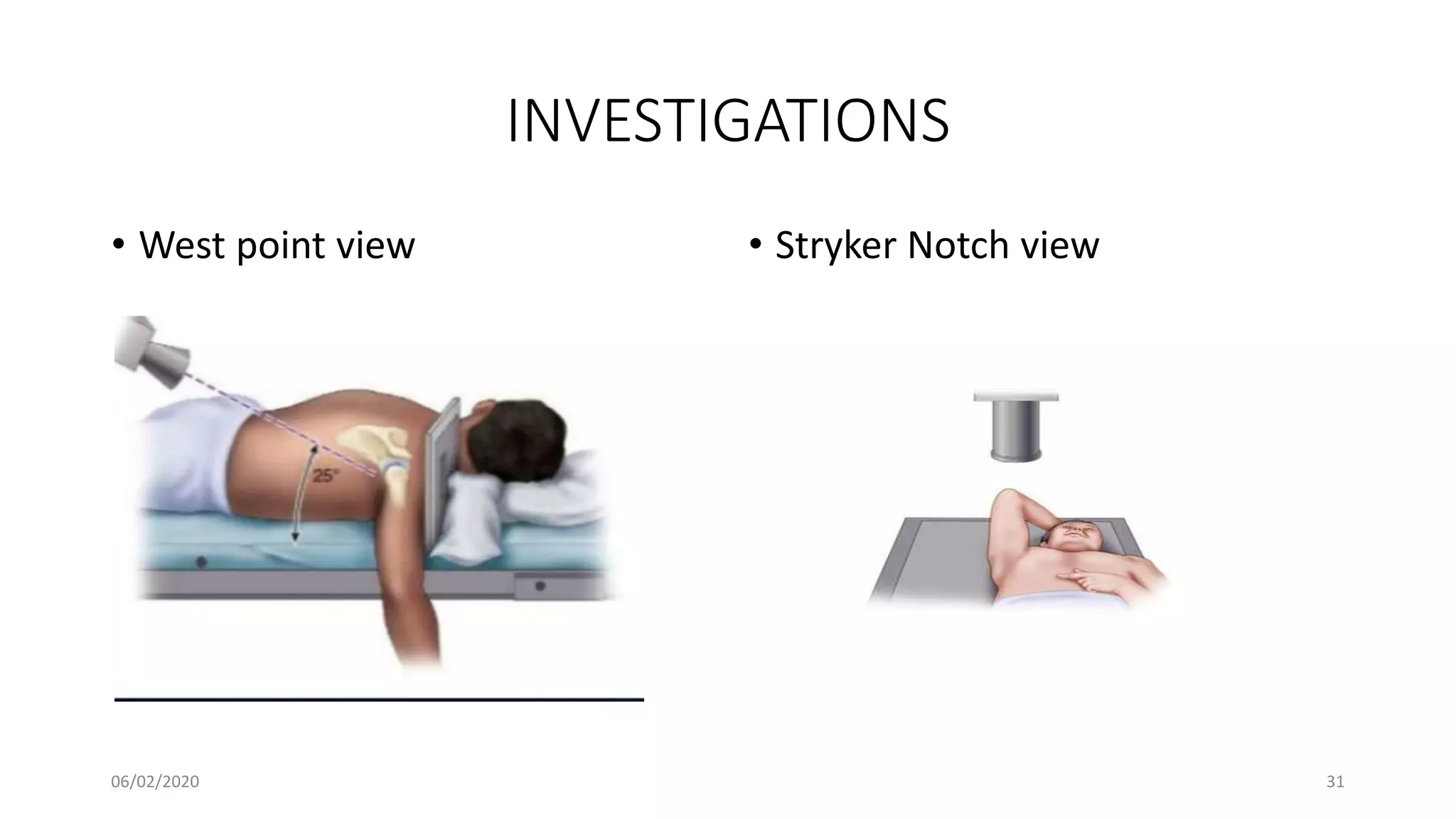
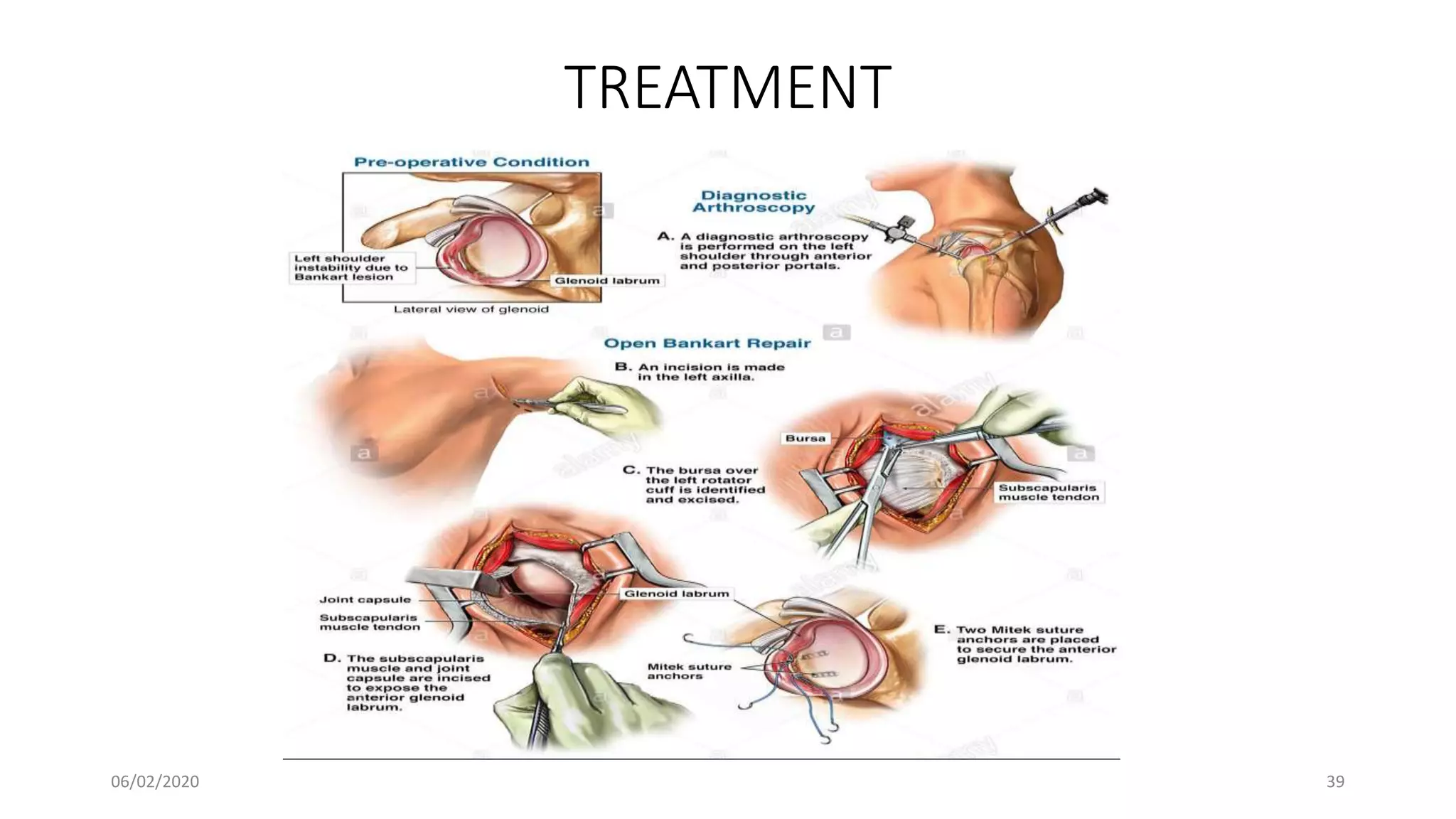
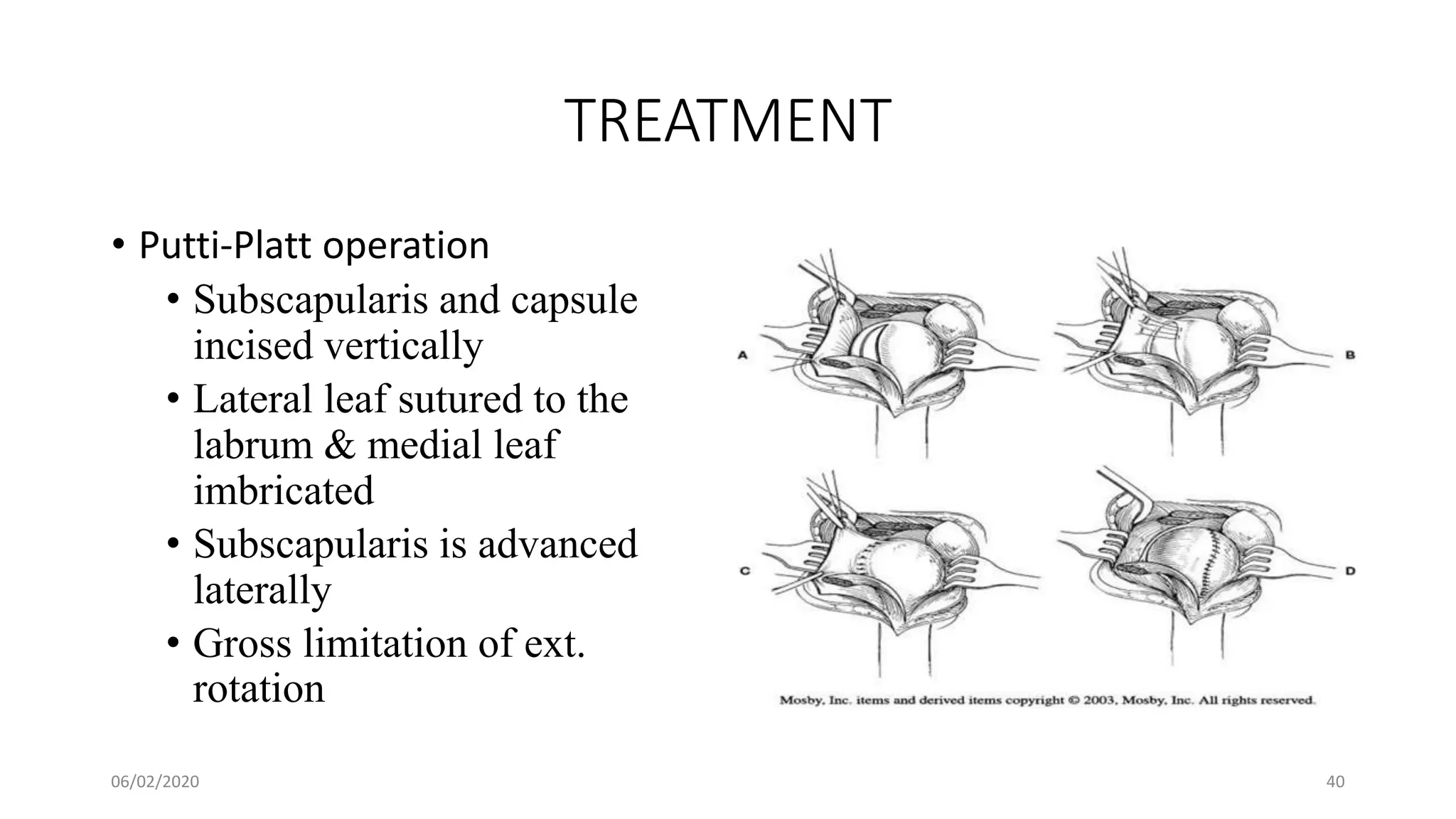
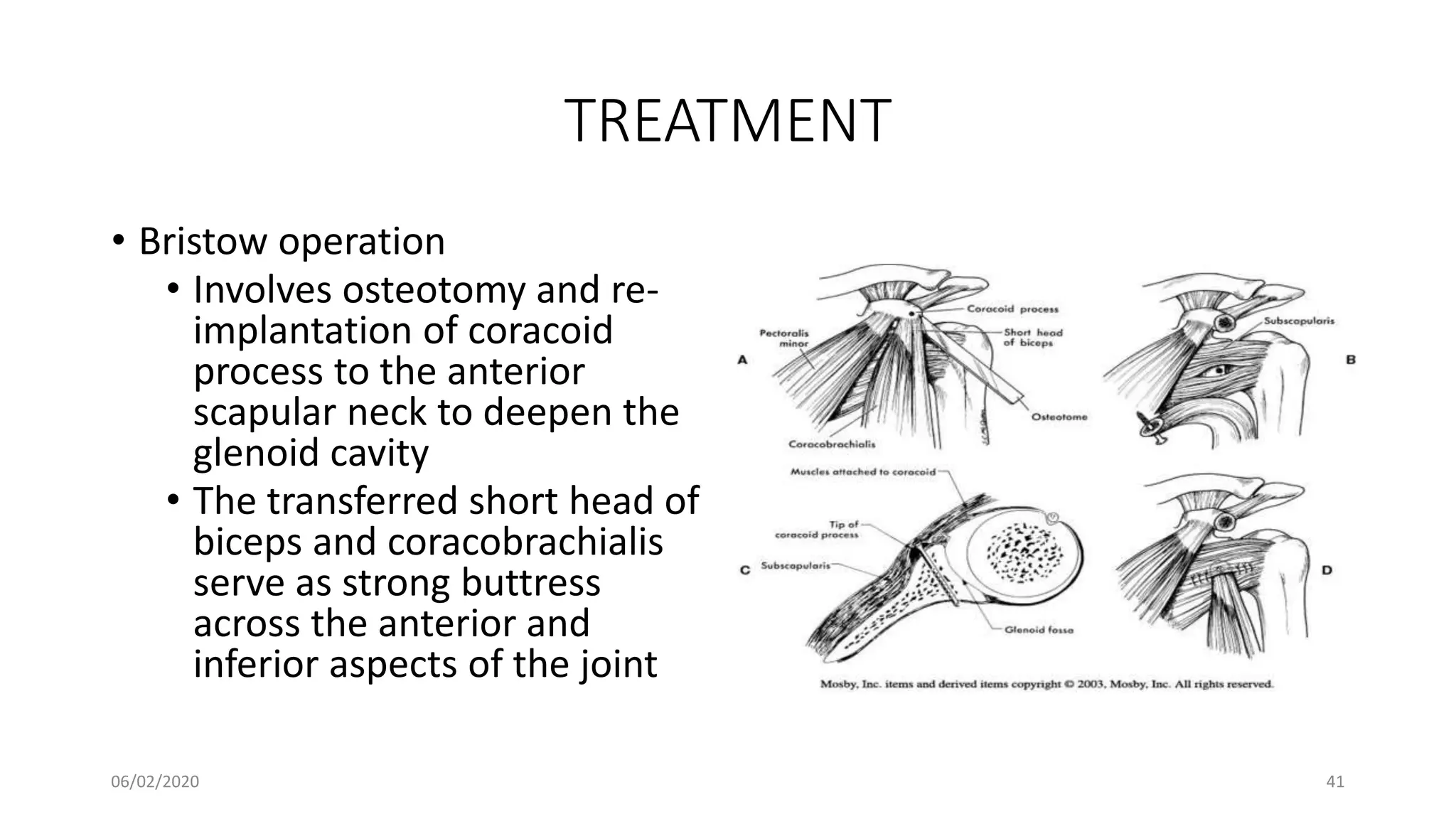
This document discusses the pathology and management of recurrent shoulder dislocations. It begins with an introduction covering the epidemiology and risk factors for recurrence. It then covers the surgical anatomy of the shoulder joint and stabilizing structures. The main pathological findings associated with recurrence include Bankart lesions, Hill-Sachs lesions, and ligamentous laxity. Treatment involves both surgical and non-surgical options depending on the individual case. The most common surgical procedures are Bankart repair and Latarjet procedure. Post-operative rehabilitation is important for recovery. Recurrence rates can be reduced with proper identification and treatment of the underlying causes.