This document discusses the epidemiology, pathogenesis, and diagnosis of irritable bowel syndrome (IBS). Some key points include:
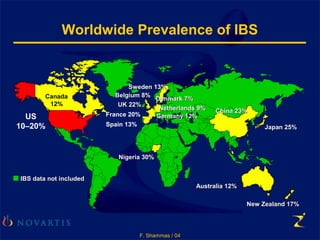
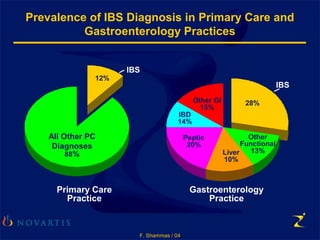
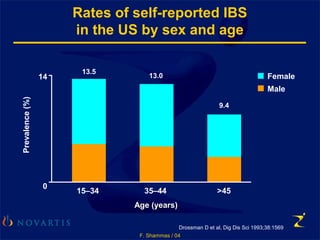
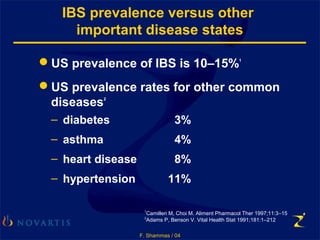
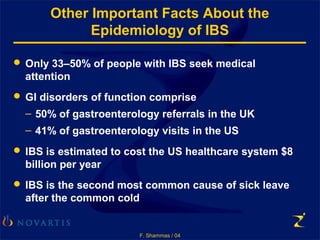
- IBS affects 10-20% of the population worldwide and is more common in females. Onset is usually in early adulthood.
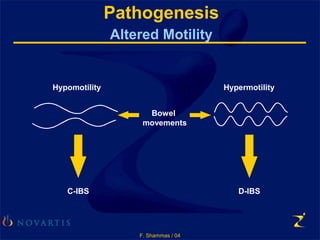
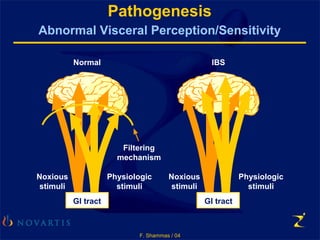
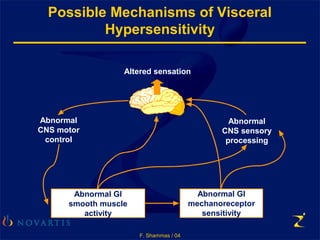
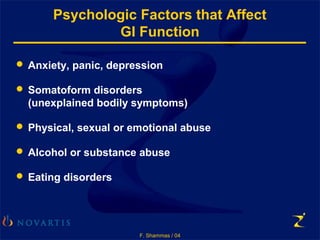
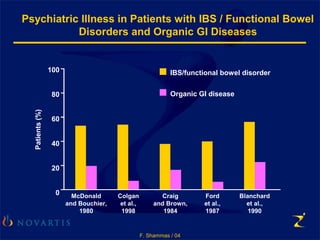
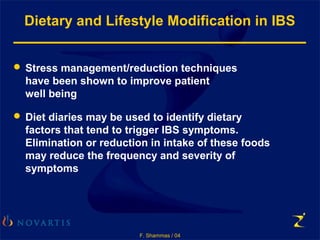
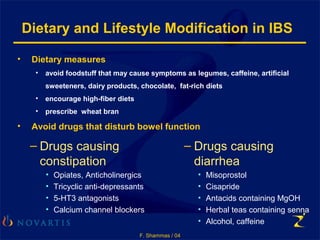
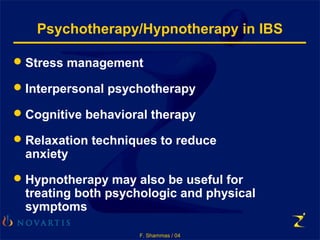
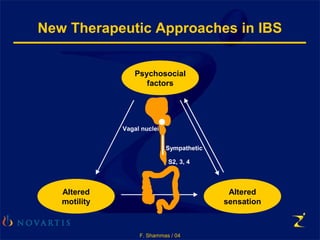
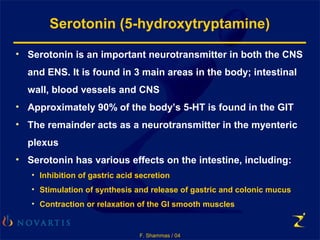
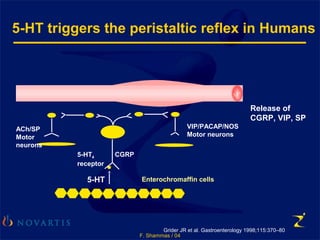
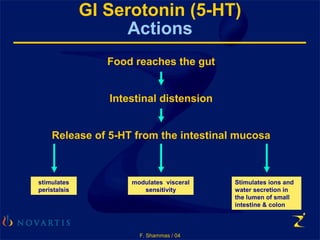
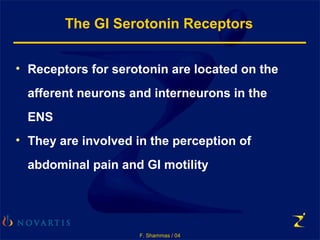
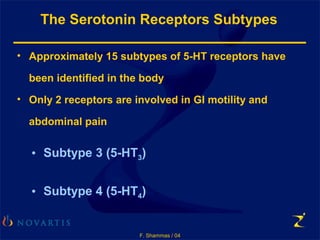
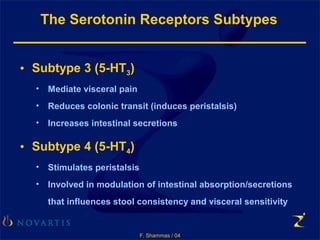
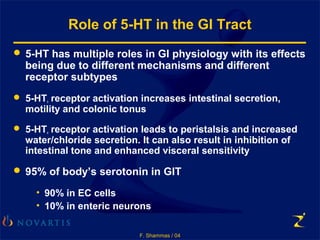
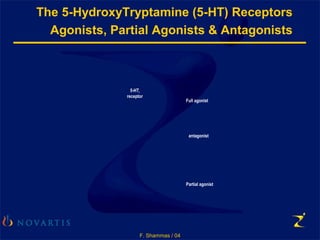
- The cause is poorly understood but involves altered intestinal motility and abnormal visceral sensitivity. Factors like diet, medication use, stress, and hormones can trigger symptoms.
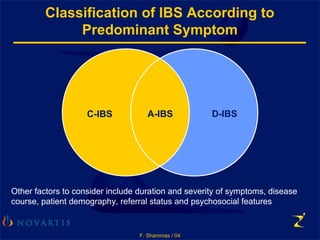
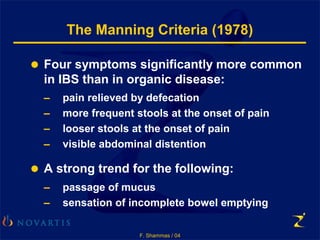
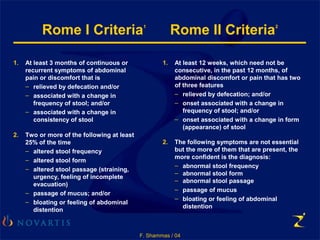
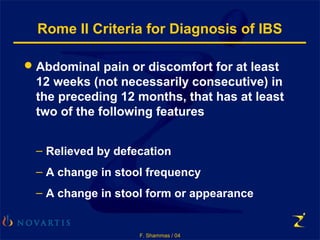
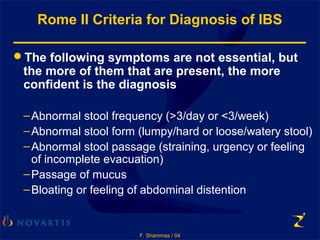
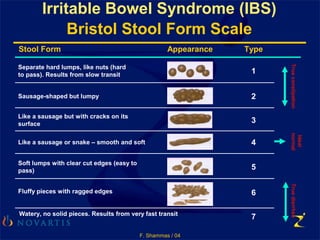
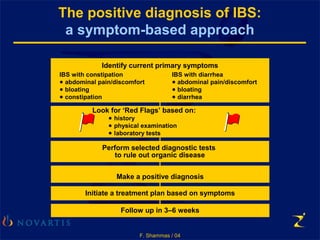
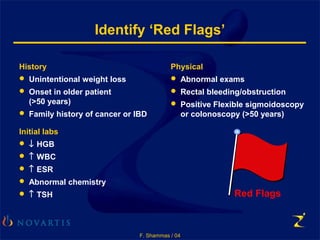
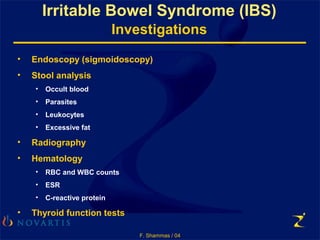
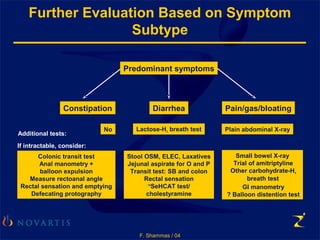
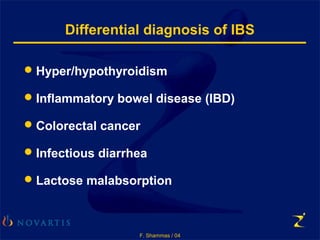
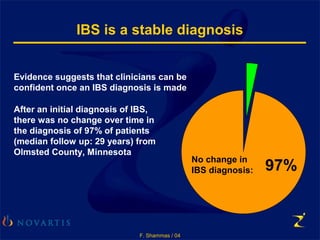
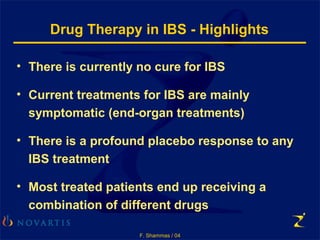
- Diagnosis is based on symptoms meeting the Rome criteria of abdominal pain relieved by defecation and associated with changes in stool frequency or form. Testing aims to rule out other organic causes.
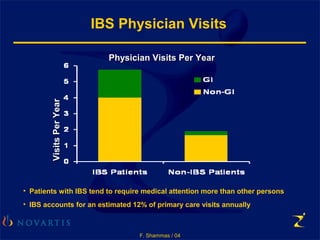
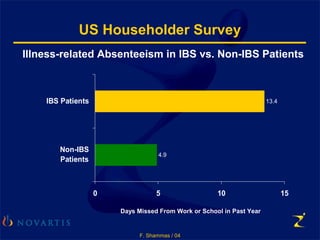
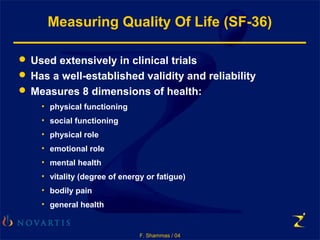
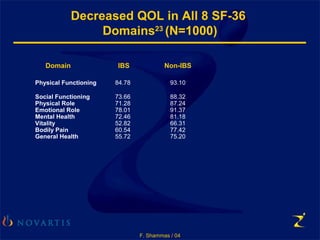
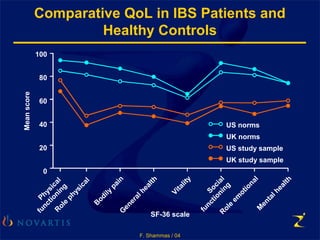
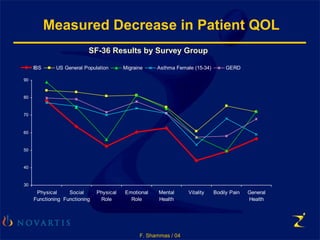
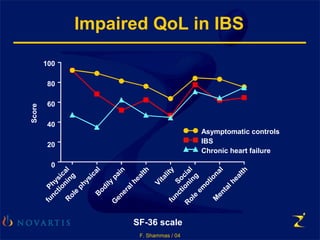
- IBS decreases patients' quality of life by interfering with daily activities and functioning