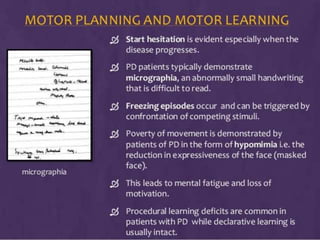
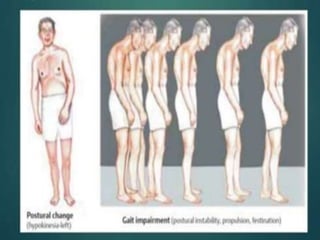
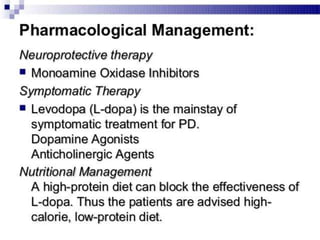
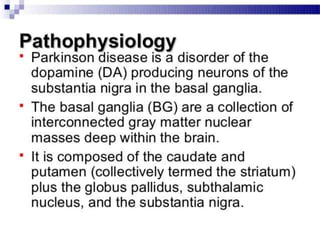
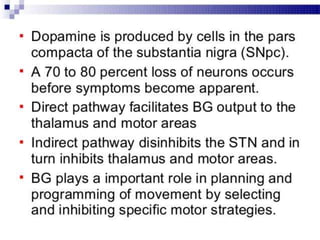
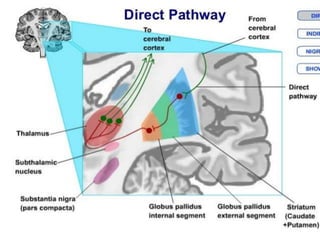
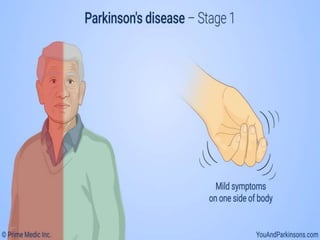
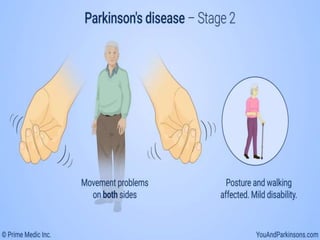
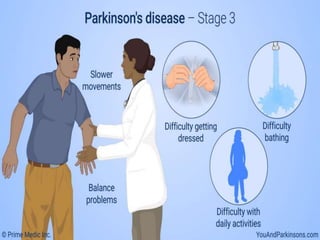
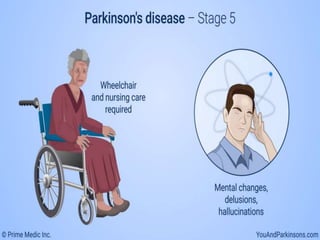
Parkinson's disease is a progressive nervous system disorder that affects movement. It is characterized by motor symptoms like rigidity, bradykinesia, tremor, and postural instability. Non-motor symptoms can also occur and include loss of smell, sleep disturbances, mood changes, and others. While the cause is largely unknown, both genetic and environmental factors are involved. Treatment focuses on managing symptoms through medication and other therapies. As the disease progresses, symptoms worsen and disability increases.
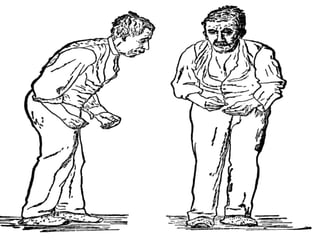


![• Akinesia refers to a poverty of spontaneous
movement.
• For example, the patient with PD
demonstrates hypomimia or masked facial
expression, with significant social
consequences.
• The absence of associated movements (e.g.,
arm swing during walking) or freezing (e.g.,
sudden stops in movement as in freezing of
gait [FOG] ) are other examples.
• Freezing episodes can be triggered by
confrontation of competing stimuli.](https://image.slidesharecdn.com/pd-200625134227-200702100836/85/Parkinsons-disease-38-320.jpg)