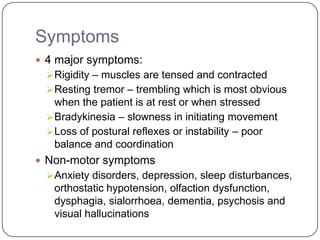
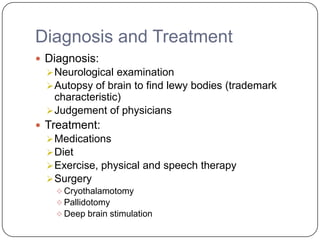
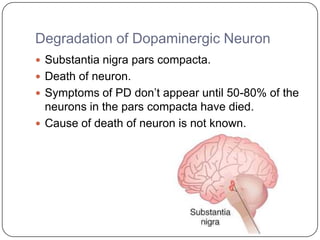
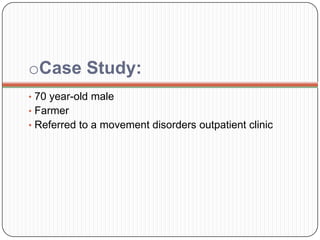
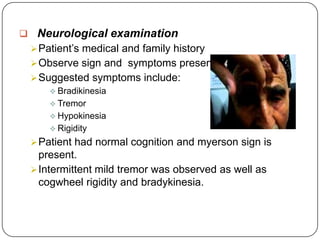
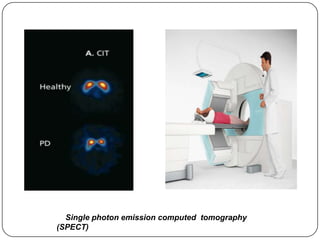
Parkinson's disease is a progressive neurological disorder that results from the loss of dopamine-producing neurons. The document discusses the causes, symptoms, diagnosis and treatment of Parkinson's disease. It presents a case study of a 70-year-old male farmer diagnosed with the disease. His symptoms included tremors, rigidity and bradykinesia. He was diagnosed through neurological exams and SPECT imaging. His treatment plan included starting levodopa and dopamine agonists to manage his symptoms.
![Reference
Anonymous. (2012). Tremor Fact Sheet. [Online]. Available from:
http://www.ninds.nih.gov/disorders/tremor/detail_tremor.htm.Nati
onal, Institute of Neurological Disorders and Stroke. Accessed on
2nd March 2013
Dr Ananya Mandal, MD. (2013). Parkinson's Disease
Pathophysiology. [Online]. Available from: http://www.news-
medical.net/health/Parkinsons-Disease-Pathophysiology.aspx.
[Accessed on 1st March 2013].
Dr. Ananya Mandal. (2013). Parkinson’s disease Prognosis.
[Online]. Available from: http://www.news-
medical.net/health/Parkinsons-Disease-Prognosis.aspx.
[Accessed on 2nd March 2013].
Malaysian Parkinson’s Disease Association. (2012). Association
wants Disability Rights for Parkinson’s Patients. [Online].
Available from:
http://mpda.org.my/article.php?type=news&9ja847hd0a1=144.
[Accessed on 2nd March 2013].](https://image.slidesharecdn.com/parkinsonsdisease-130926201959-phpapp02/85/Parkinson-s-disease-31-320.jpg)
![Mayo Clinic. Parkinson’s Disease: Risk Factors. [Online]. Available
from: http://www.mayoclinic.com/health/parkinsons-
disease/DS00295/DSECTION=risk-factors. [Accessed on 1st
March 2013].
Parkinson’s Disease Society. The professional’s guide to
Parkinson’s Disease. [Online]. Available from:
http://www.parkinsons.org.uk/pdf/B126_Professionalsguide.pdf.
[Accessed on 1st March 2013].
Parkinson’s UK. Types of Parkinson’s and parkinsonism. Online].
Available from:
http://www.parkinsons.org.uk/about_parkinsons/what_is_parkins
ons/types_of_parkinsons.aspx. [Accessed on 2nd March 2013].
Public Health and Genetics Information Series. Parkinson’s
disease. [Online]. Available from:
http://www.hgen.pitt.edu/counseling/public_health/parkinsons.pdf
. [Accessed on 1st March 2013].
Robert A Hauser, MD. (2013). Parkinson Disease . [Online].
Available from : http://emedicine.medscape.com/article/1831191-
overview#aw2aab6b2b1aa.[Accessed 1st March 2013].](https://image.slidesharecdn.com/parkinsonsdisease-130926201959-phpapp02/85/Parkinson-s-disease-32-320.jpg)
![Takashi Hanakawa. (1999). Mechanisms underlying gait
disturbance in Parkinson's disease. [Online]. Available
from :
http://brain.oxfordjournals.org/content/122/7/1271.full.
[Accessed on 2nd March 2013]
Ted K Koutouzis, MD. (2005). Parkinson's Disease.
[OnlineAvailable from :
http://www.emedicinehealth.com/parkinson_disease/article
_em.htm. [Accessed 1st March 2013].
University of Maryland Medical Centre. Diagnosing
Parkinson’s Disease. [Online]. Available from:
http://www.umm.edu/parkinsons/diagnosis.htm. [Accessed
on 1st March 2013].
Wooten. G.F., Currie. L.J., Bovbjerg. V.E., Lee.J.K. and
Patrie. J. (2013). Are men at greater risk for Parkinson’s
disease than women? J Neurol Neurosurg Psychiatry.
75:637-639.](https://image.slidesharecdn.com/parkinsonsdisease-130926201959-phpapp02/85/Parkinson-s-disease-33-320.jpg)