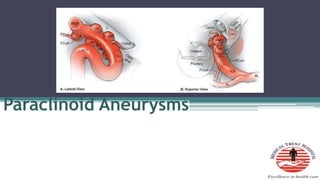
Paraclinoid aneurysms
- 2. • Introduction • Anatomy • Classification • Indications for Treatment • Pre-op evaluation • Management techniques
- 3. Paraclinoid aneurysms • Nutik • Arise from the ICA distal to the cavernous sinus but proximal to the PCoM • 5 – 10% of all intracranial aneurysms arise from this segment of the ICA
- 4. • Female preponderance - 9:1(Shimizu et al; AJNR 2016) • High incidence of being multiple • Rupture rate is lower than supra-clinoid aneurysms • Half of pts with C6 segment aneurysms have additional intracranial aneurysms elsewhere
- 6. Seven segments • Cervical – C1 • Petrous – C2 • Lacerum – C3 • Cavernous – C4 • Clinoid – C5 • Ophthalmic – C6 • Communicating/Terminal segment – C7
- 9. C5 and C6 segments • Clinoid segment ▫ Optic strut ▫ ACP ▫ Superiorly – DR ▫ Inferiorly – COM ▫ Interdural • Ophthalmic segment ▫ Sub-arachnoid space ▫ Ophthalmic artery ▫ Sup Hypophyseal artery
- 12. Anterior Clinoid process • Cline – Greek – bed • Lesser sphenoid wing • Superior orbital fissure • Optic canal • Cavernous sinus
- 16. • Carotid sulcus • Infra-clinoid carotid groove
- 17. Dural reflections off ACP • Falciform ligament ▫ Covers posterior optic canal • Dural ring ▫ Superior dural surface fuses with ICA adventitia ▫ Distal dural ring ▫ Diaphragma sellae • Carotid-oculomotor membrane(COM) ▫ Periosteal dura ▫ Marks exit of ICA from C.S
- 21. Distal Dural ring • Slopes down ▫ Anterior to posterior ▫ Lateral to medial • Medial to ICA - subarachnoid recess – Carotid cave
- 23. Carotid cave • Kobayashi(1989) • Sup – Medial surface of DR • Lat – Medial wall of ICA • Medially – Carotid groove • Cave communicates with the clinoidal venous plexus • Subarachnoid space • 3 patterns ▫ Slit (34%) ▫ Pocket(24%) ▫ Mesh(10%)
- 24. • Carotid collar attaches to ICA only at Upper dural ring • Space between collar and ICA – Clinoid venous plexus • Lower ring – Perneczky’s ring
- 25. • Middle clinoid process • Osseous bridge • Carotico-clinoidal foramen
- 26. Neural relationship • Optic Nerve ▫ Optic canal ▫ Optic strut ▫ Falciform ligament
- 28. Arterial bends - 2 • 1st ▫ Sharp posterior turn ▫ Superior vector stress on the anterior and dorsal wall • 2nd ▫ Medial to lateral curve ▫ Stress on the medial aspect
- 30. Branch points • Ophthalmic artery ▫ Dorso-medial ICA surface ▫ Just above DR ▫ Infero-lateral to Optic nerve ▫ Optic canal
- 32. • Superior hypophyseal artery ▫ Largest perforator from Ophthalmic segment ▫ Runs medially ▫ Optic chiasm ▫ Optic tracts
- 34. Barami classification(2003) • Type Ia – Arising from the ophthalmic segment of the ICA and related to the ophthalmic artery • Type Ib – arising from the superior ophthalmic segment but without relationship with ICA branches • • Type II – from ventral ophthalmic segment of ICA without ICA branches relation
- 36. • Type IIIa – from medial ophthalmic segment of the ICA and related to the SHA • Type IIIb – from the medial clinoid segment below the DR • Type IV –Large aneurysms involving the clinoid and the ophthalmic segment of the ICA • Ia – Most common - 43%
- 37. • Clinoidal segment ▫ Antero-lateral variant ▫ Medial variant • Ophthalmic segment ▫ Ophthalmic artery aneurysms ▫ Sup Hypophyseal artery aneurysms ▫ Dorsal variant • Carotid cave aneurysms • Transitional aneurysms
- 39. Anterolateral variant • From anterolateral surface of C5 • Superior projecting towards ACP • Erode optic strut – visual loss
- 40. Medial variant • From medial surface of clinoidal segment • Enlarges towards sella and sphenoid sinus • Expands beneath the diaphragma sellae into the pituitary fossa • Hypopituitarism • Visual loss • Rupture - Simulate apoplexy
- 46. Ophthalmic artery aneurysms • From posterior bend of ICA just distal to origin of Ophthalmic artery and DR • Project dorsally or dorsomedially • Can elevate the Optic nerve against the falciform ligament
- 47. • Monocular inferior nasal field defect • Entire nasal field • Superior temporal field loss in C/L eye
- 48. Large ophthalmic artery aneurysms • Thickened or calcified walls • Antero-inferior portion
- 49. Superior hypophyseal artery aneurysms • Medial surface of ICA • Just distal to the DR • Surrounded by Superior hypophyseal artery perforators • Can project into the carotid cave – unlikely to rupture when small
- 51. • When it fills the cave and extends into the suprasellar region – Risk of hemorrhage rises • Thickening or calcification along the anterior medial aspect near the origin • Giant aneurysms – compress chiasm like pituitary tumors
- 52. Dorsal variant aneurysms • Dorsal aspect of ICA • Distal to ophthalmic artery origin • Blisters • Hemorrhage when small and expand as fusiform lesions externally • Very fragile
- 54. Carotid cave aneurysms • Arises proximal to ophthalmic artery • Below distal dural ring • Points ventromedially into the cave
- 55. Clinical presentation • Sudden severe headache • Decreased visual acuity/field defects • Changes in colour vision • Diplopia • Panhypopituitarism • Pituitary apoplexy • Epistaxis • Facial numbness
- 56. Indication for treatment • Small <1cm asymptomatic clinoid segment aneurysms – conservative • Small symptomatic lesions (visual deficits, focal unrelenting headaches) – Rx • Lesion whose protective ACP roof has been removed - Rx • >1cm – often extend into subarachnoid space – Increased risk of rupture – Rx even if asymptomatic
- 57. • Ophthalmic segment aneurysms – low risk of rupture. Expn – dorsal variant • All symptomatic aneurysms > 1cm – Rx • Large or giant lesions – Flow diverters
- 58. Pre-operative evaluation • Cranial nerve deficits ▫ Visual acuity and fields ▫ EOM ▫ Facial sensations • Endocrine status • DSA • CT angiography – DR can be identified. Atheroma + calcifications • Anterolat v/s Ophthalmic in CT ▫ Erosion of ACP ▫ Proximal origin ▫ Dorsolat v/s dorsomedial ▫ Angiographic waist
- 59. Clinoidal medial Sup Hypophyseal • Projects medially • Originates below diaphragma sellae • Superior surface is flattened by the diaphragma • Narrow neck(b/w DR and COM) • Projects medially • Originates above diaphragma sellae • Not flattened • Wide neck
- 61. • EVD or Lumbar drain • Positioned supine with a shoulder roll ipsilateral to the lesion • Head is elevated above the heart • Rotated 45 to 60 degrees away from the side of the aneurysm
- 62. • Cervical carotid exposed • Skin incision • Pterional craniotomy with an orbital osteotomy • Lesser wing is removed extra-durally down to the base of ACP
- 64. Anterior clinoidectomy • Extradural – Dolenc approach • Intradural approach • Intradural advantage – visualisation of aneurysm throughout the procedure
- 65. Extradural ACP removal -EDAC • Avoid extradural ACP removal if a clinoidal segment anterolateral variant is suspected • Extend medial dissection • Diamond drill • Dural attachments released
- 68. Intradural ACP removal • Basal removal • Dura opened in a curvilinear fashion • Sylvian fissure split • Aneurysm, ICA and optic apparatus visualised
- 70. • Falciform ligament sectioned • Better visualization of optic apparatus and aneurysm • Optic canal – unroofed • Optic strut drilled down • Optic nerve sheath - sectioned
- 72. • DR sectioned circumferetially • ICA can me mobilized
- 74. Techniques • Temporary proximal cervical carotid ligation • Trapping of aneurysm • Intra-aneurysmal suction decompression • Fenestrated clips – calcified lesion • ICG – perforator patency • Intraoperative angiography
- 75. Clinoidal segment • Anterolateral variant – gently curved or side angled clip parallel to the anterolateral surface of ICA • Medial variant
- 76. Ophthalmic segment • Calcification along anterior aspect • Sup Hypophyseal - Right angled fenestrated clip • Dorsal wall aneurysms ▫ Blister variety – Clipping after trapping ▫ Sling of fascia or PTFE – wrap and clip
- 84. Complications • Delayed stenosis or thrombosis • Post-operative visual deterioration – 8.7% (Nanda and Javalkar et al – Neurosurgery 2011) • Heat from drilling • Manipulation of Optic nerve • Perforators • Most patients have improved visual function after surgery(De Oliveira et al – Neurosurg Focus 2009)
- 85. • 3rd, 4th, 6th nerve palsies • Avoid excessive cranial nerve manipulation or cavernous sinus packing • CSF rhinorrhea – ACP drilling – Yo –Yo technique
- 87. • Detachable coils • Stenting and flow diverters • Balloon assisted coiling • Adjunct to surgery – Suction decompression + Intraop angiography
- 88. Complications • Coil compaction – refilling of aneurysm • Blockage of parent vessel • Progression of aneurysm thrombosis to parent vessel • Embolization of aneurysm thrombus
- 90. PED v/s Coiling v/s Clipping(JNS 2018 – Michael A silva et al) • PED has highest rate of visual improvement – 93% • Complication rates 9% - PED • Complete occlusion – Clipping(97) > PED(89) > Coiling(78)
- 91. • CN palsy – 29% clipping > 13% PED > 0% coiling • SHA – coiling • Ophthalmic – clipping • Large aneurysms – PED and coiling
- 92. Bibliography • Youmans • Ramamurthi • 7 Aneurysms