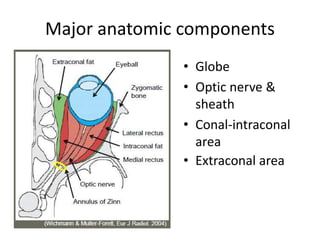
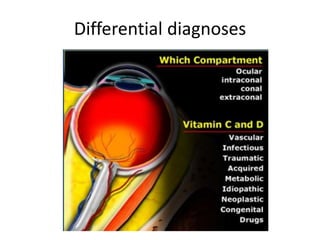
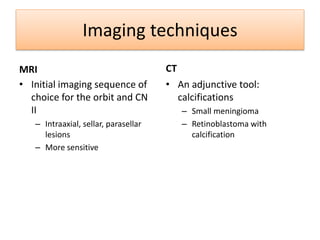
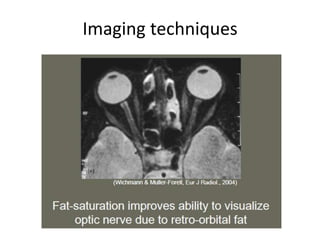
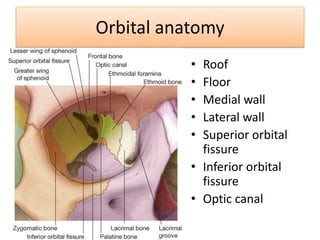
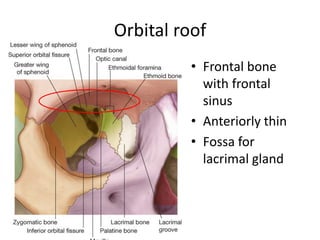
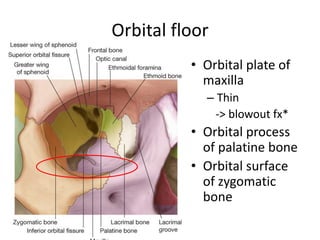
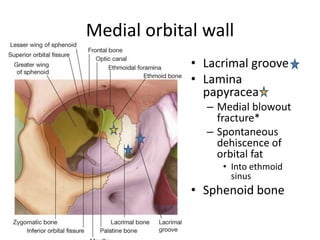
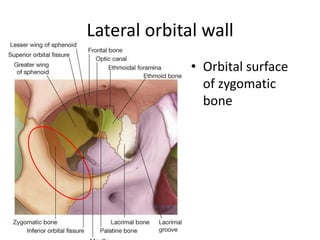
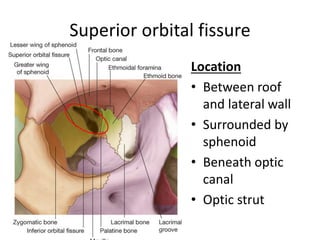
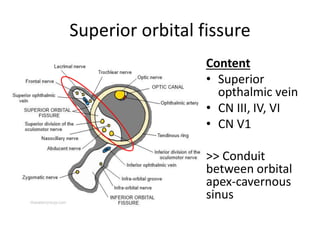
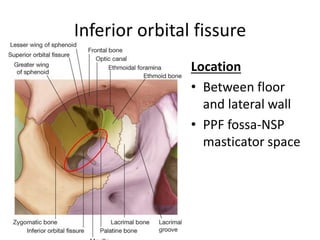
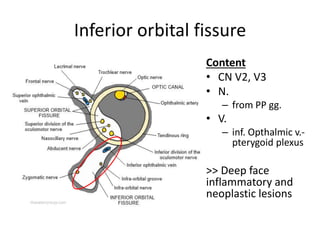
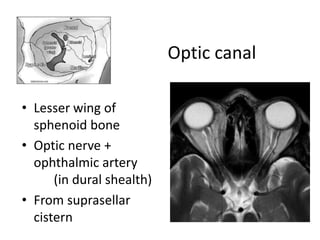
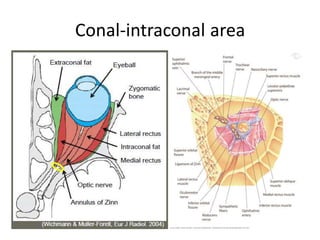
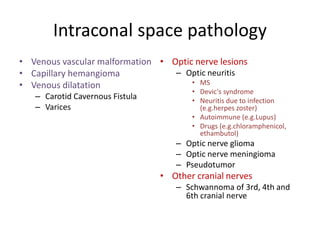
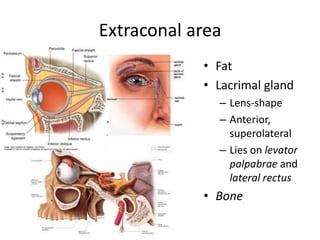
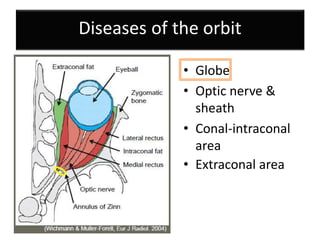
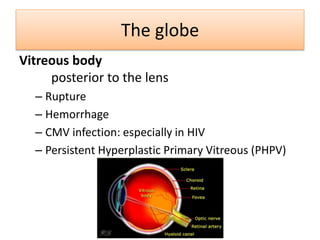
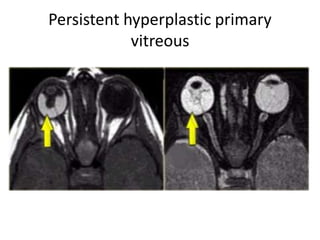
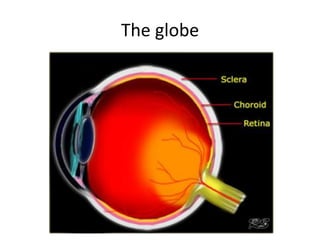
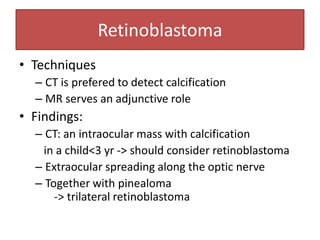
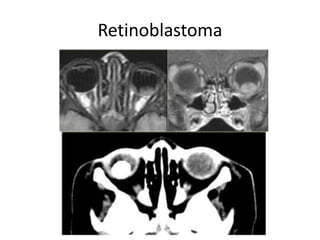
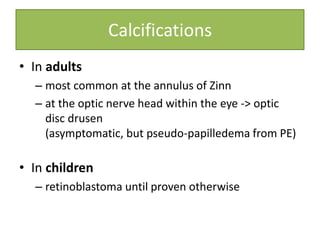
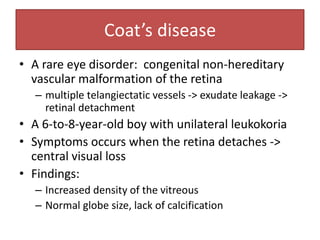
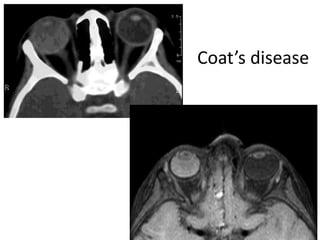
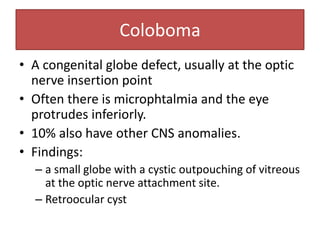
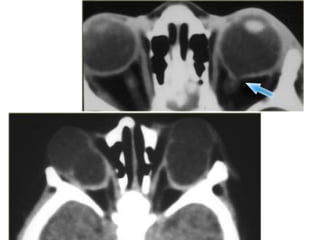
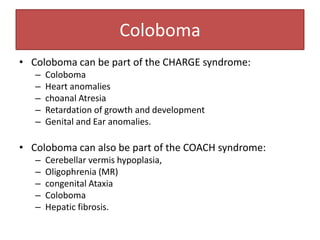
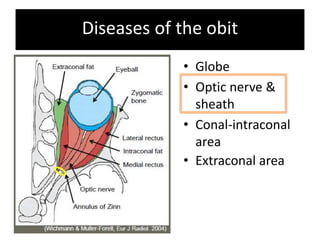
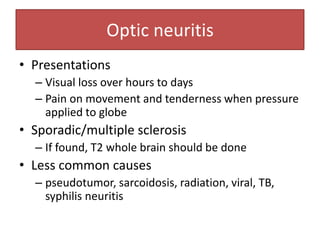
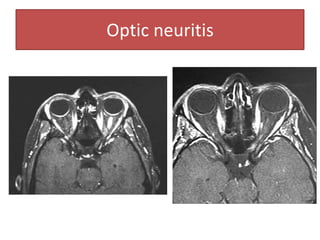
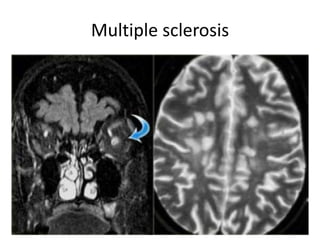
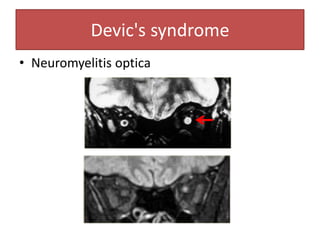
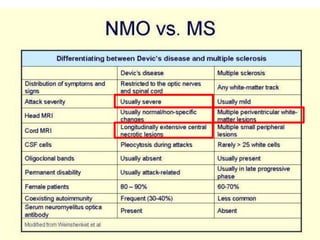
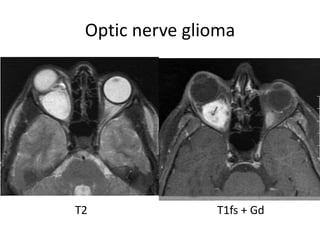
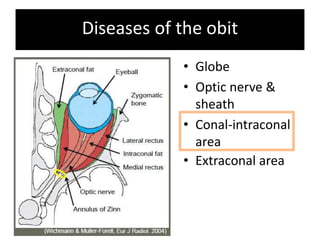
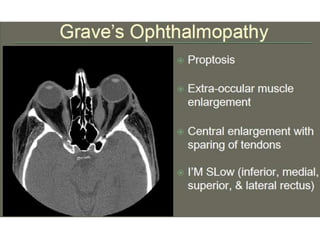
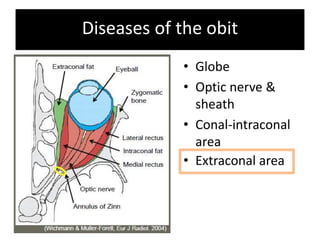
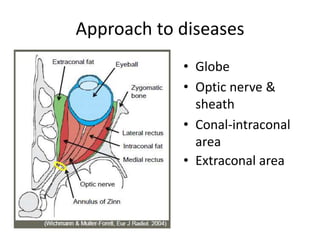
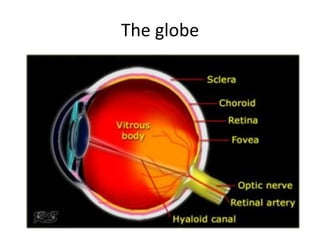
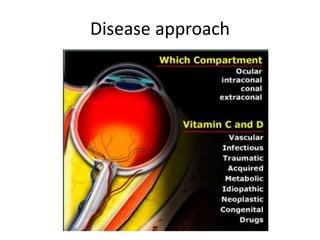
This document provides an overview of orbital anatomy and diseases. It describes the major anatomic components of the orbit including the globe, optic nerve, extraconal and intraconal areas. Common pathologies are discussed for each anatomic structure, such as retinoblastoma affecting the globe and optic neuritis involving the optic nerve. Imaging techniques for evaluating the orbit including MRI and CT are also reviewed. Key anatomical structures like the superior orbital fissure and its contents are defined.