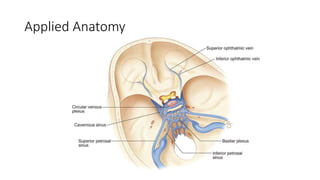
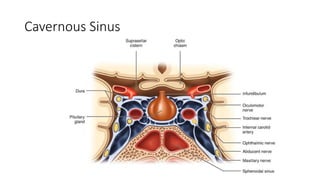
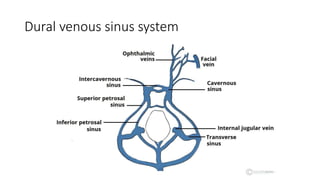
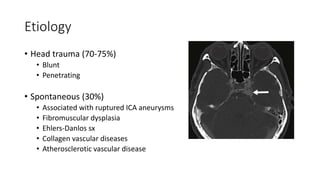
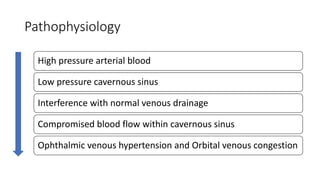
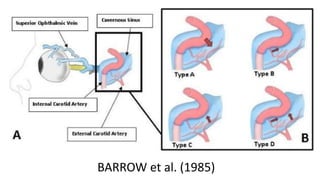
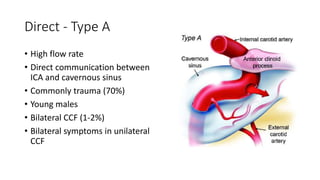
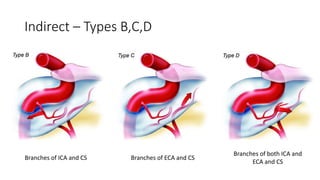
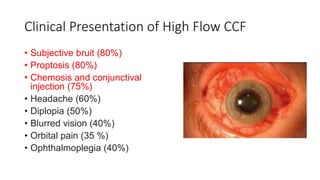
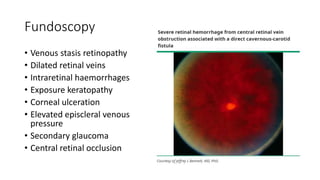
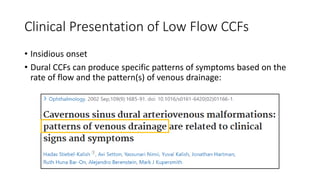
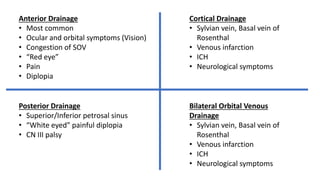
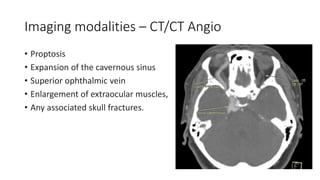
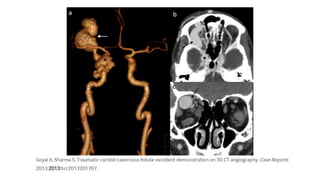
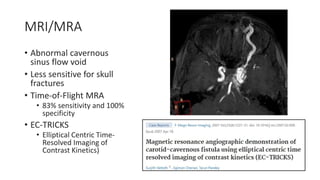
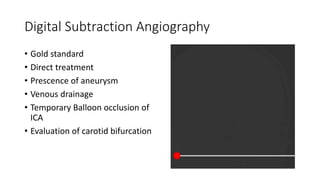
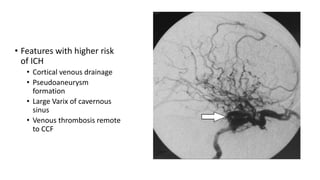
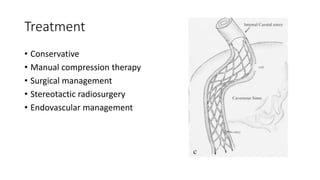
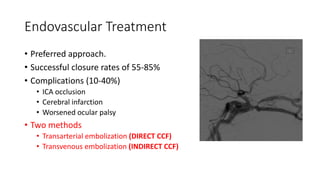
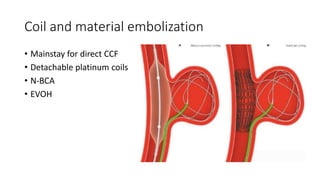
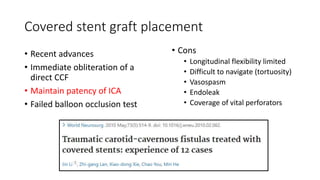
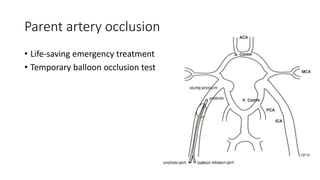
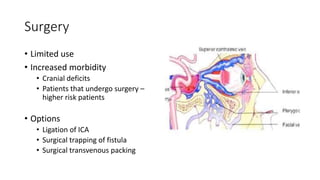
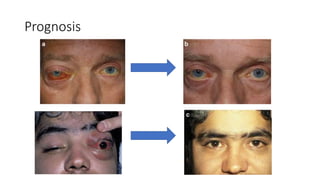
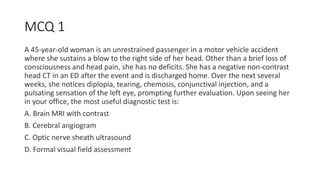
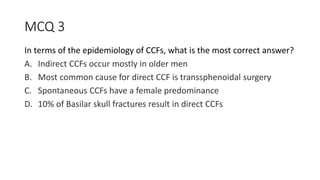
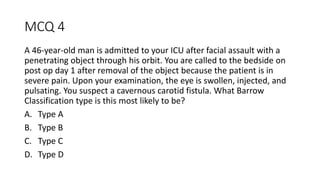
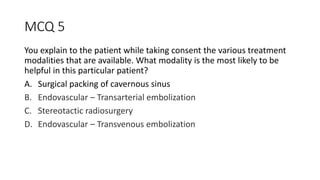
This document provides information on carotid-cavernous fistulas (CCFs). It discusses the anatomy of the cavernous sinus and pathophysiology of CCFs. It notes that CCFs represent 12% of dural arteriovenous fistulas. The majority are caused by trauma, especially in young males, while spontaneous CCFs occur more in older females. Clinical presentation depends on flow rate, with high flow direct CCFs causing eye symptoms and low flow indirect CCFs having insidious onset. Treatment options include conservative management, endovascular embolization, and radiosurgery, with the approach depending on fistula type and symptoms.