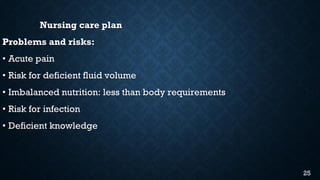
Pancreatitis is inflammation of the pancreas that can be acute or chronic. Acute pancreatitis has a sudden onset of abdominal pain and is often caused by gallstones or alcoholism. Chronic pancreatitis results in permanent destruction of the pancreas through progressive inflammation and fibrosis. The nursing care plan focuses on managing the patient's acute pain, risk for infection, imbalanced nutrition due to decreased intake, and providing health education on risk factors, diet, and symptoms of diabetes.

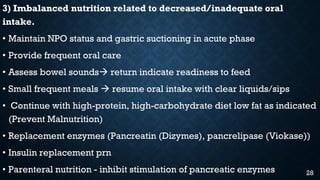
![5) Deficient knowledge due to absence or deficiency of cognitive
information related to specific topic.
• Educate patient and his/her family on his condition and prognosis
• Educate on risk/causative factors: excessive alcohol intake,
gallbladder disease, hyperlipidemia, some drugs (Zidovudine,
sulfonamides, oral contraceptives etc)
• Diet: low fat and low protein
• Encourage cessation of alcohol and smoking, assist with rehabilitation
• Educate on signs and symptoms of Diabetes Mellitus (3Ps)
**** WHAT HEALTH EDUCATION ARE YOU GOING TO GIVE TO
THIS PATIENT? [10 marks]****
30](https://image.slidesharecdn.com/pancreatitis-200407082714/85/Pancreatitis-30-320.jpg)