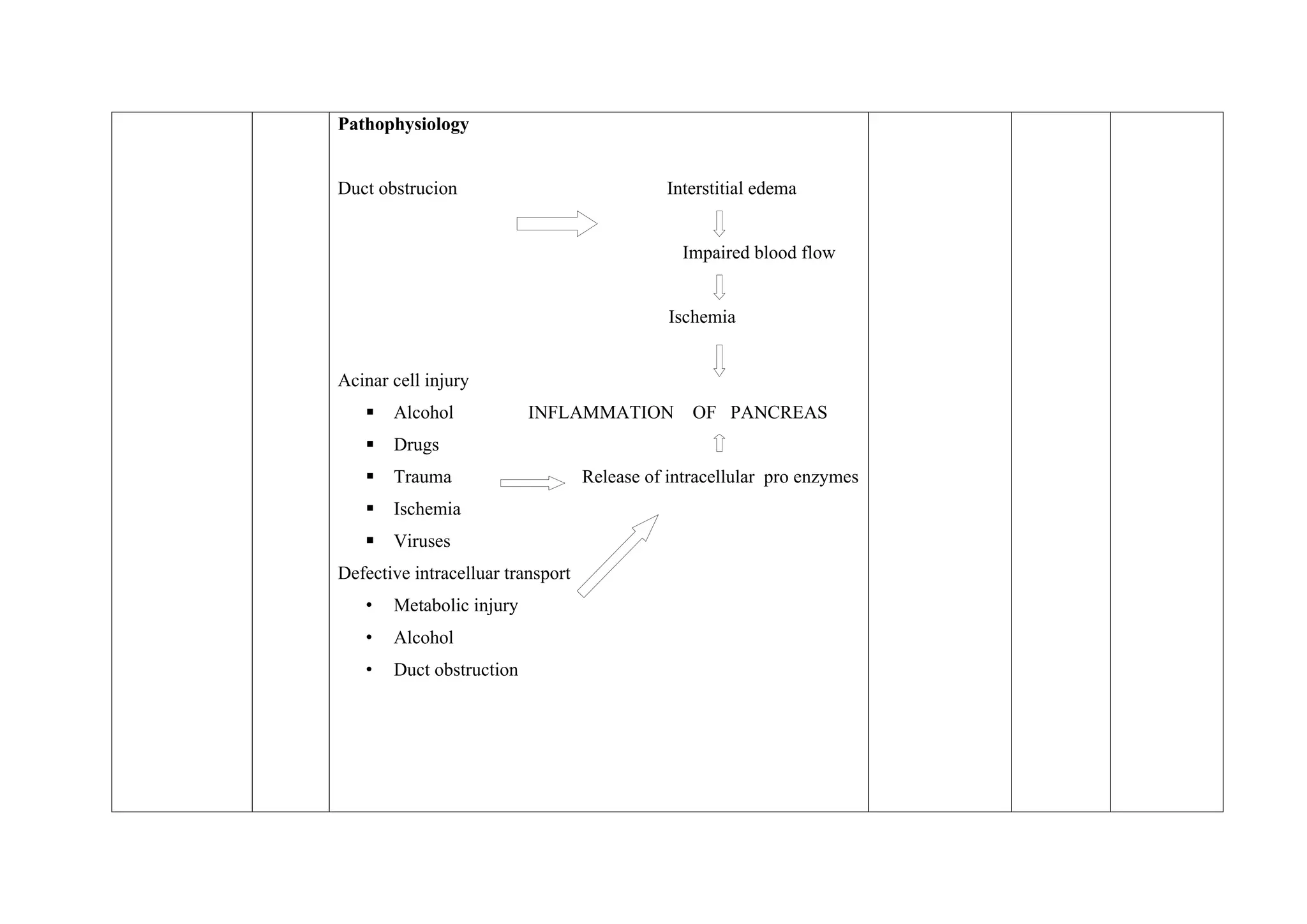
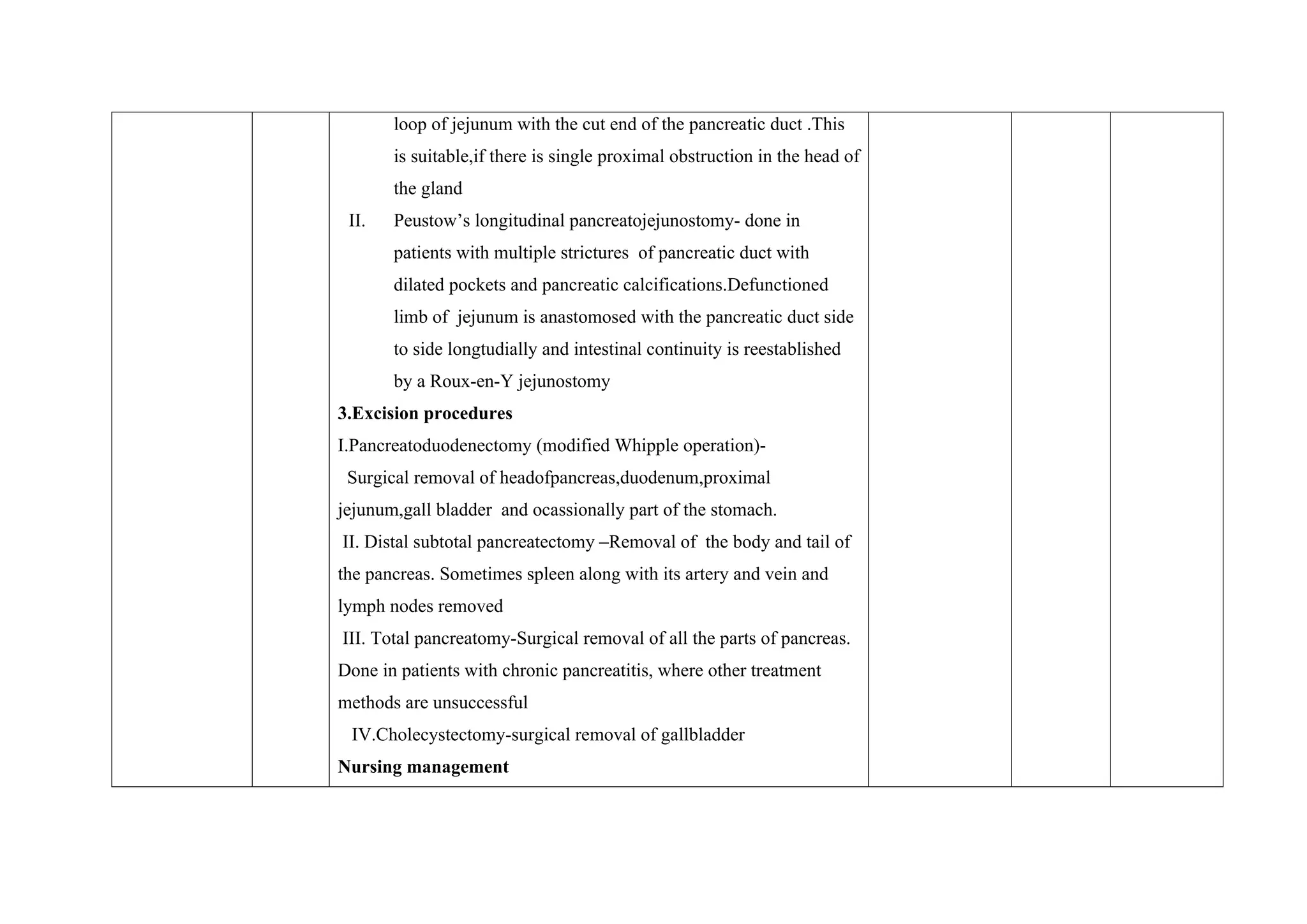
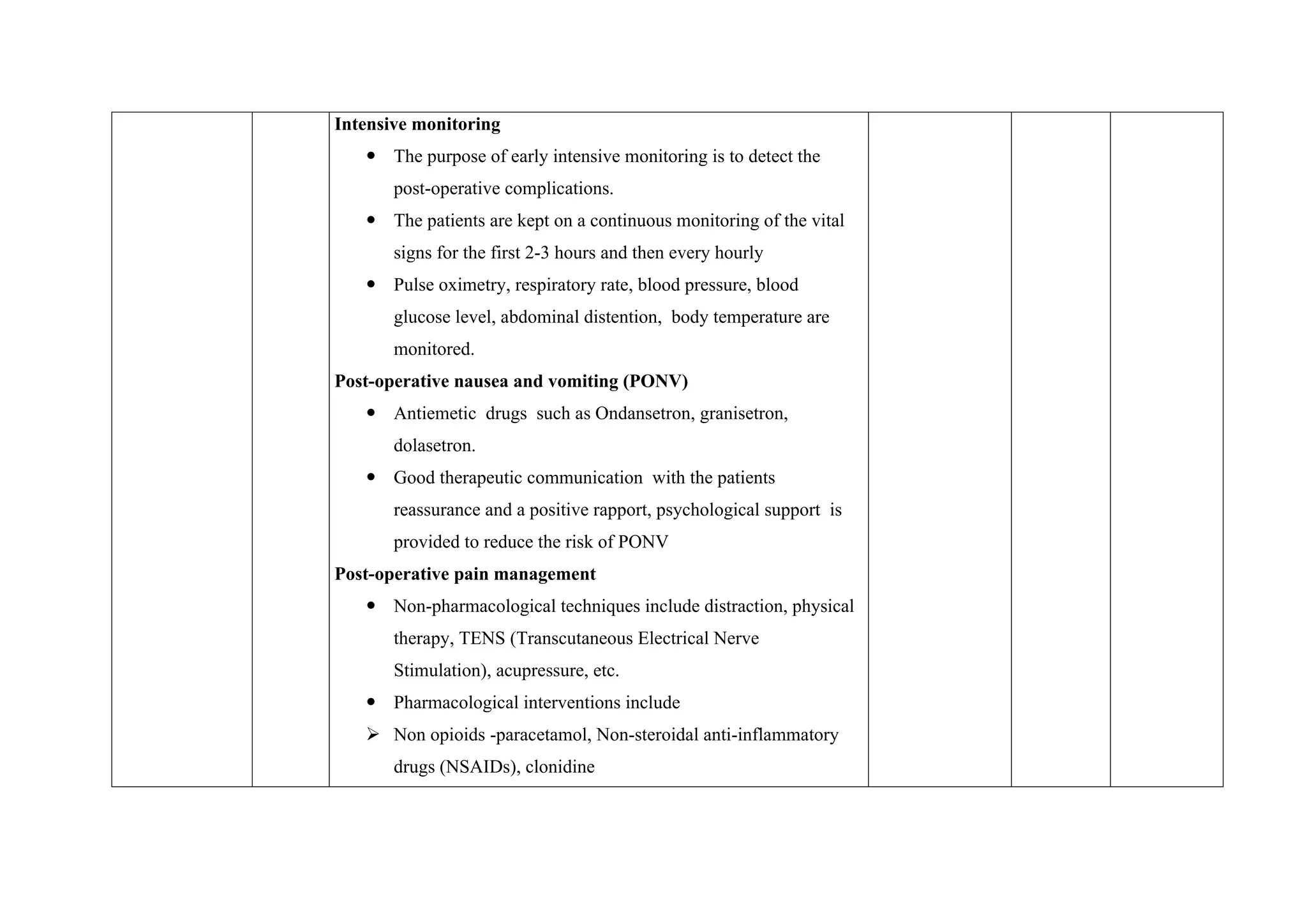
This document outlines a comprehensive lesson plan focused on pancreatitis, covering its definitions, classifications, causes, pathophysiology, clinical features, diagnosis, management, surgical options, nursing care, and post-operative considerations. It details both conservative and surgical management strategies for pancreatitis, as well as the nursing care required before and after surgery, ensuring proper nutrition, fluid balance, and pain management. Lastly, it emphasizes the importance of patient education for ongoing care and monitoring post-surgery.