The document discusses pancreatitis, including:
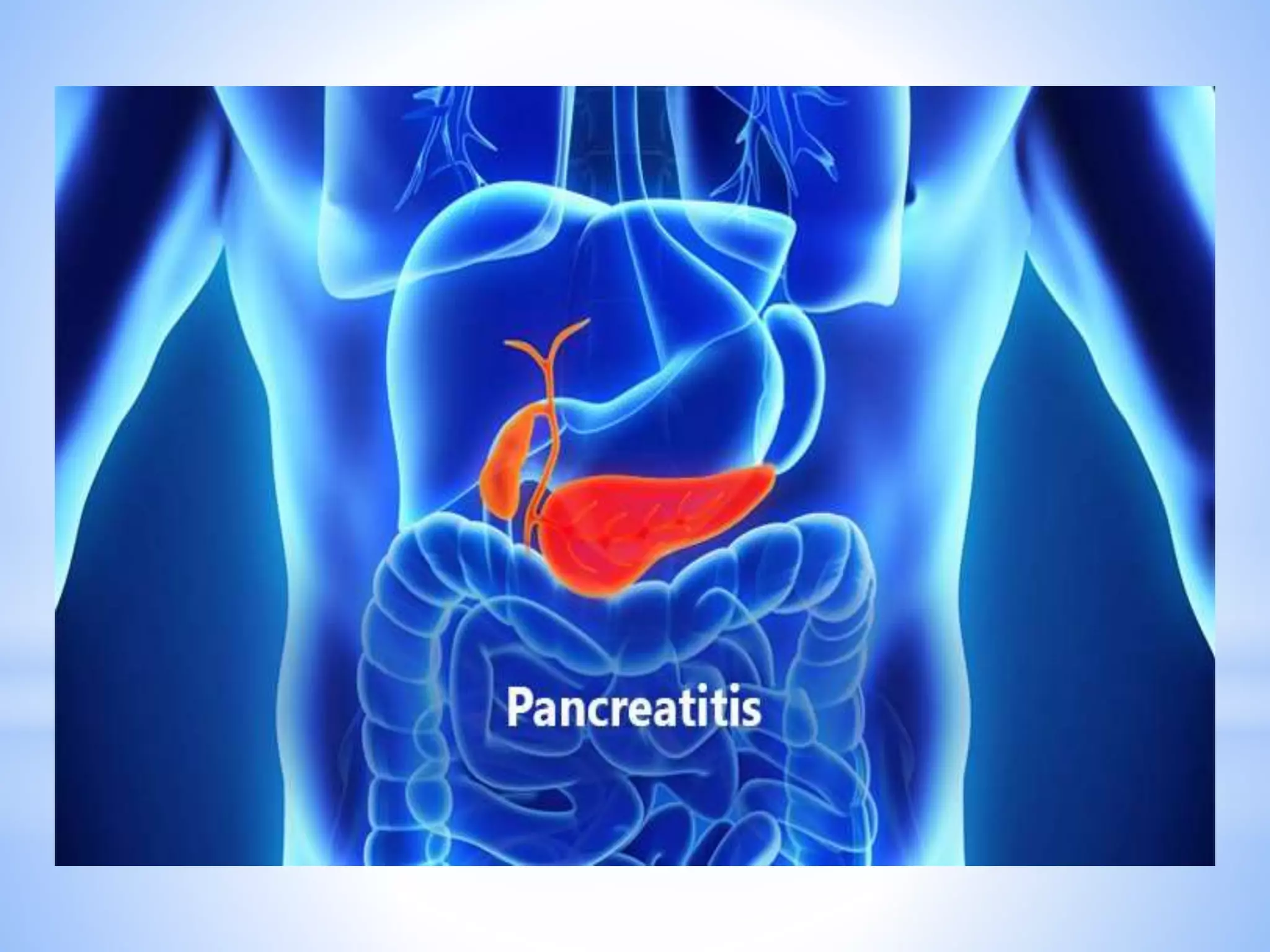
1. The pancreas is an organ that secretes enzymes and hormones. It can become inflamed due to premature activation of enzymes within the pancreas.
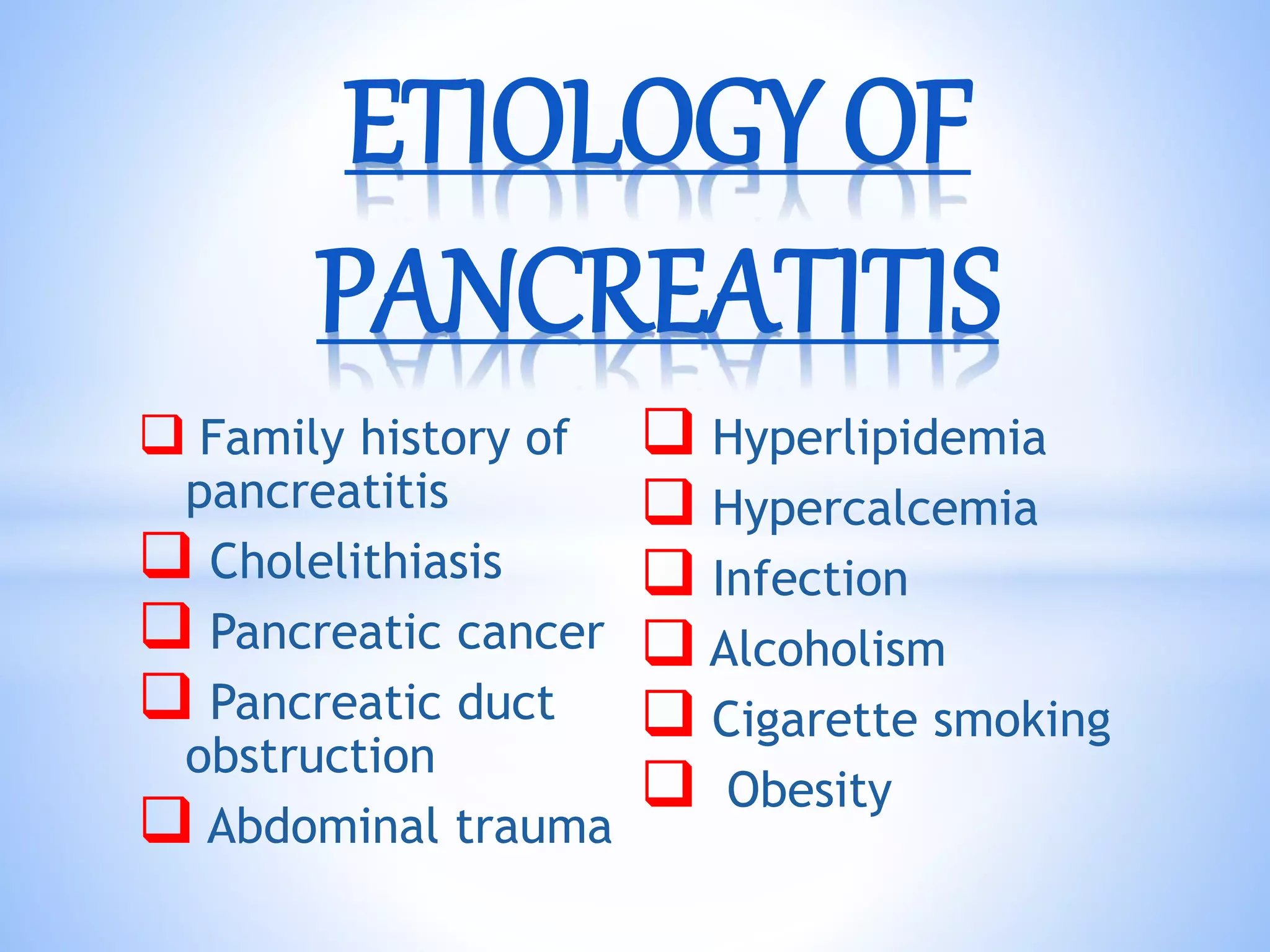
2. Pancreatitis can be acute or chronic. Acute pancreatitis ranges from mild to severe and is often caused by gallstones or alcohol use. Chronic pancreatitis involves permanent damage from long-term inflammation.
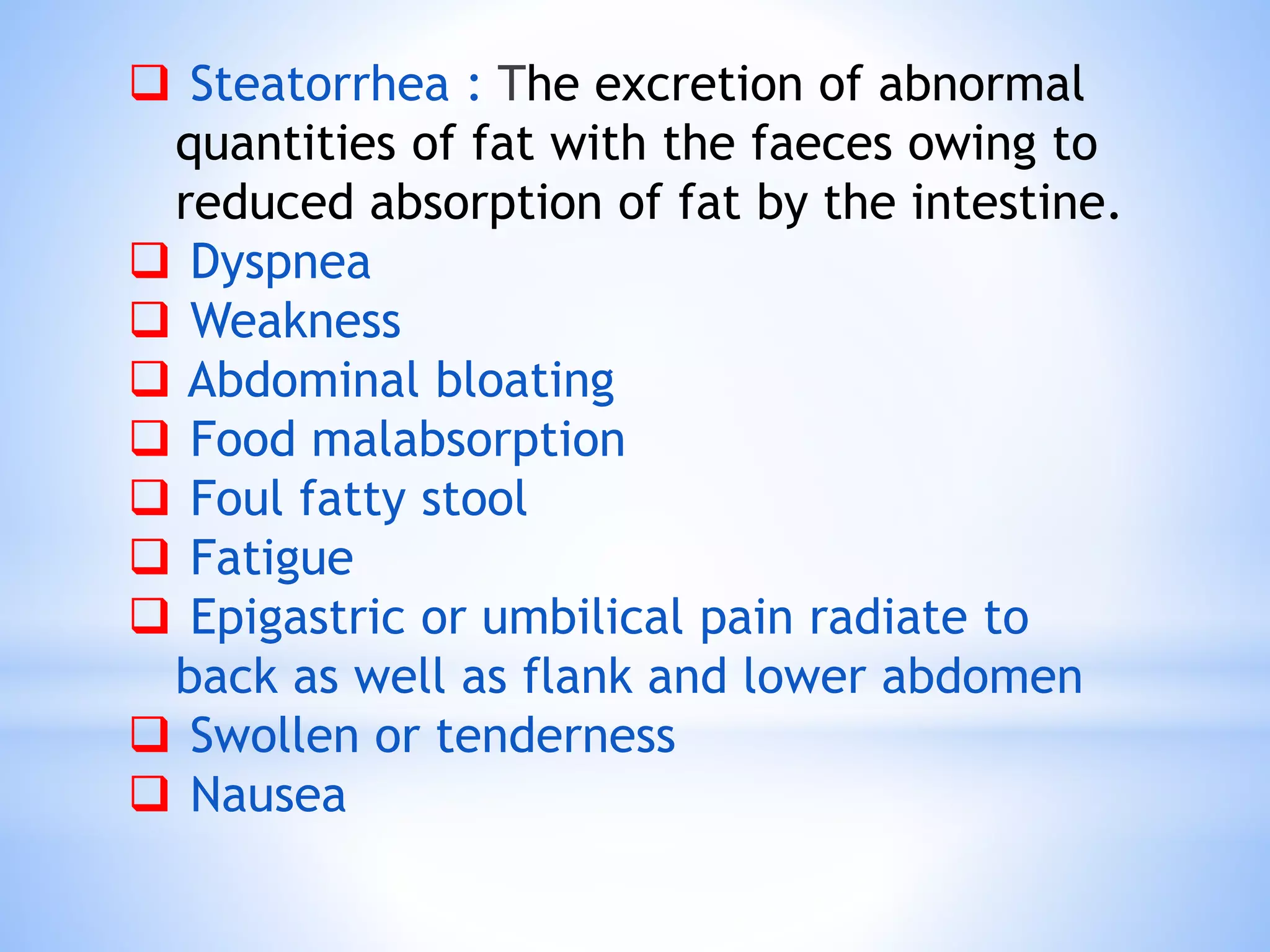
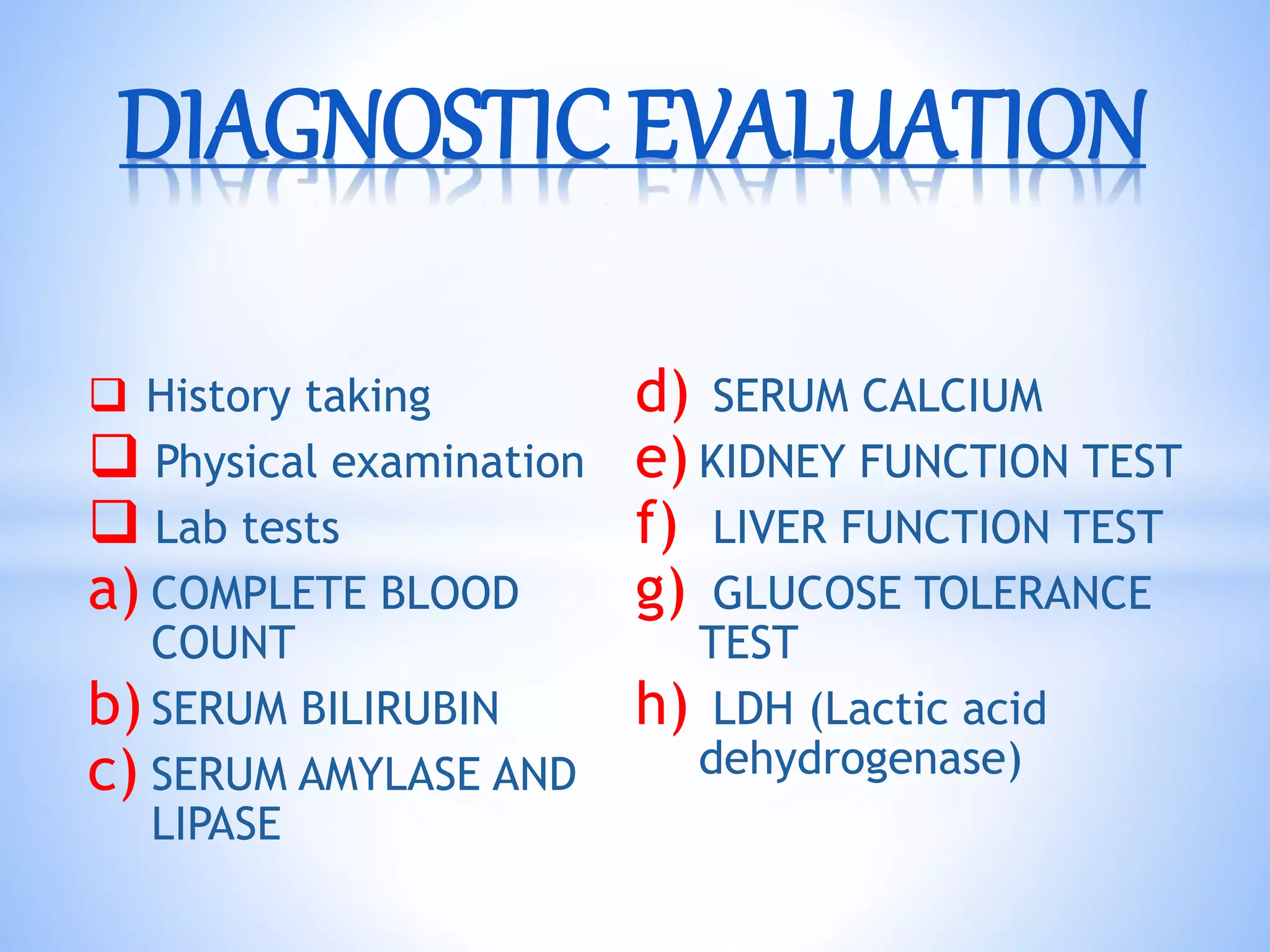
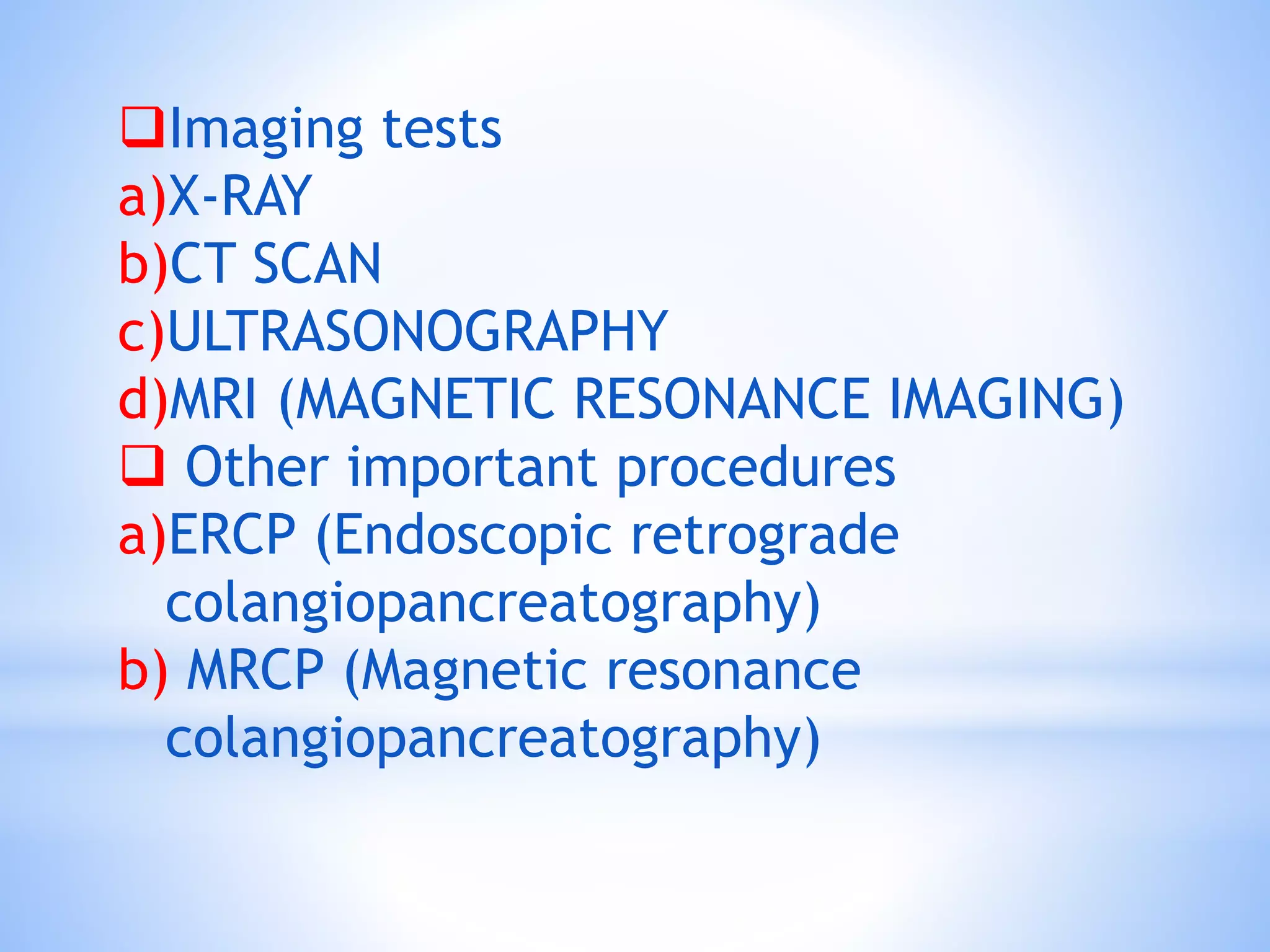
3. Symptoms include abdominal pain, vomiting, and digestive issues. Diagnosis involves blood tests, imaging, and procedures like ERCP. Treatment focuses on pain relief, antibiotics, nutrition, and treating complications which can include infections.