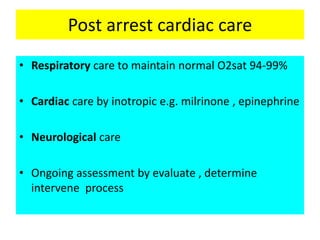
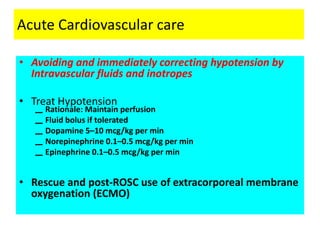
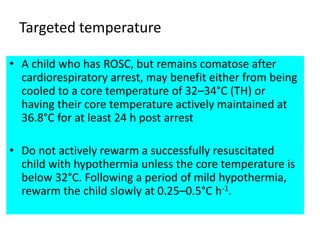
This document provides guidelines for post-arrest care in pediatric patients. It outlines recommendations for respiratory care to maintain oxygen saturation between 94-99% and use of inotropic drugs like milrinone and epinephrine for cardiac care. It also discusses guidelines for neurological care, ongoing assessment, and treatment of hypotension. Specific recommendations are provided for ventilation, drug therapies including epinephrine, dopamine, norepinephrine and factors influencing outcomes. Targeted temperature management and control of blood glucose are also addressed.