This document discusses hypertension (high blood pressure), including its definition, global prevalence, classification, risk factors, complications, treatment recommendations, and prevention strategies. Some key points include:
- The global prevalence of hypertension was estimated to be 26.4% in 2000 and is expected to exceed 30% by 2025.
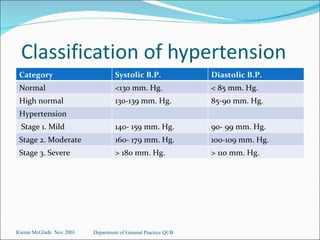
- Hypertension is classified into stages based on systolic and diastolic blood pressure readings, ranging from normal to severe.
- Risk factors include age, family history, obesity, diet, smoking, and physical inactivity.
- Complications can include damage to the heart, blood vessels, brain, kidneys, and other organs if left untreated.
- Treatment involves lifestyle changes and may require