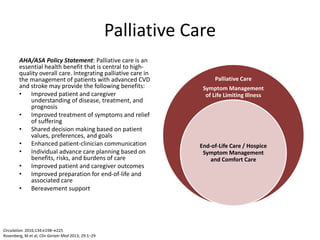
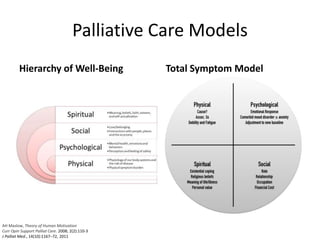
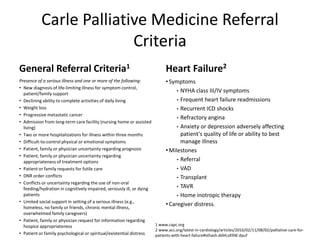
Palliative care is an essential health benefit that enhances overall care for patients with advanced cardiovascular disease (CVD) and stroke by improving communication, symptom management, and decision-making. Referral criteria include serious illnesses, physical or emotional symptoms, and caregiver distress among others. Effective communication about palliative care should focus on its role in managing symptoms and supporting patients and families through the progression of the disease.
![Communicating About Palliative Care
What NOT to say!
• “There’s nothing left to
do…let’s have palliative care
see you.”
There is always something to
do for the patient even if there
is nothing left to treat the
disease.
What to say!
• “Palliative care works with me, your
cardiologist, to better manage your [pain,
shortness of breath or other symptom
(anxiety, fatigue, nausea)]. They are
experts in looking at this holistically and
make a comprehensive plan for how best
to relieve your [symptom].
• They can answer some of the questions
you may have about what to expect in
future as your [disease] worsens.
• They help me formulate a treatment plan
that is based on what is important to you
and what is going on with your family.
• There is support staff at the clinic who
works with the palliative care providers to
help you and your family cope with these
changes and plan for the future”
J Palliat Med, 11(6):823–828, 2008.](https://image.slidesharecdn.com/17-170711234817/85/Palliative-Care-in-Cardiology-4-320.jpg)