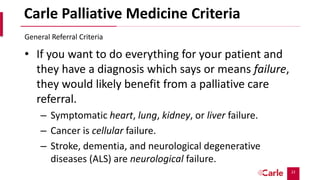
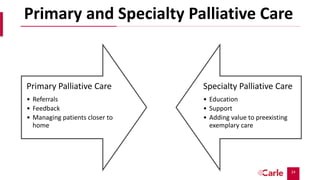
Palliative care aims to relieve suffering and improve quality of life for patients with serious illnesses and their families. It can be provided alongside curative treatment. The presentation discusses primary palliative care provided in primary care settings and specialty palliative care provided by palliative care specialists. It provides criteria for referring patients to specialty palliative care, such as advanced cancers, organ failures, neurological diseases, and frequent hospitalizations. Early referral to palliative care can improve quality of life and mood and extend survival. While many could benefit from palliative care, there are not enough specialists to meet the need.




![16
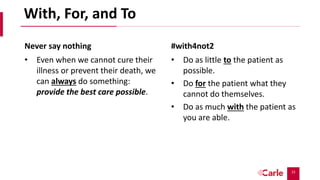
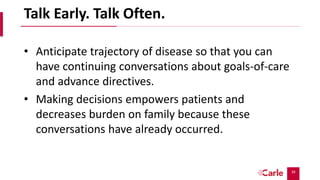
Scripting
• “Palliative care works with me, your [provider], to better manage
your [pain, shortness of breath or other symptom (anxiety,
fatigue, nausea)]. They are experts in looking at this holistically
and make a comprehensive plan for how best to relieve your
[symptom].
• They can answer some of the questions you may have about what
to expect in future as your [disease] worsens.
• They help me formulate a treatment plan that is based on what is
important to you and what is going on with your family.
• There is support staff at the clinic who works with the palliative
care providers to help you and your family cope with these
changes and plan for the future”
How to help other providers refer to palliative care](https://image.slidesharecdn.com/20-220516035404-eea3d88b/85/Primary-and-Specialty-Palliative-Care-pptx-16-320.jpg)
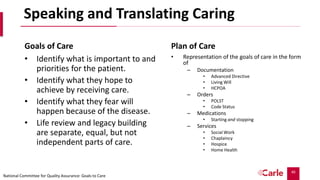
![18
Quality and Quantity
Of the 151 patients who underwent
randomization, 27 died by 12 weeks and 107
(86% of the remaining patients) completed
assessments. Patients assigned to early
palliative care had a better quality of life than
did patients assigned to standard care (mean
score on the FACT-L scale [in which scores range
from 0 to 136, with higher scores indicating
better quality of life], 98.0 vs. 91.5; P=0.03). In
addition, fewer patients in the palliative care
group than in the standard care group had
depressive symptoms (16% vs. 38%, P=0.01).
Despite the fact that fewer patients in the
early palliative care group than in the standard
care group received aggressive end-of-life care
(33% vs. 54%, P=0.05), median survival was
longer among patients receiving early
palliative care (11.6 months vs. 8.9 months,
P=0.02).](https://image.slidesharecdn.com/20-220516035404-eea3d88b/85/Primary-and-Specialty-Palliative-Care-pptx-18-320.jpg)




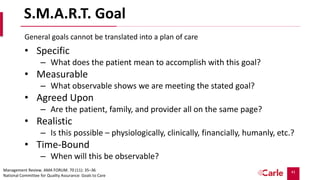
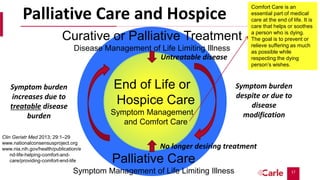
![42
Unclear Goals = Unplannable Caring
Goals of Care
• “I’m going to beat this [disease]!”
• “My family won’t let me go to a
nursing home.”
• “We’re going to fight this!”
• “I’m going to get my miracle.”
Plan of Care
• These are general, usually not agreed
upon, often unrealistic, and do not
meet a timeline consistent with life
expectancy.
• The plan of care in these case is to
explore:
– “Tell me what this means to you.”
– “Help me understand more about this
by telling me how you feel about…”
And get a family meeting with all the key
partners in the patient’s care both family
and providers.
vitaltalk.org](https://image.slidesharecdn.com/20-220516035404-eea3d88b/85/Primary-and-Specialty-Palliative-Care-pptx-42-320.jpg)