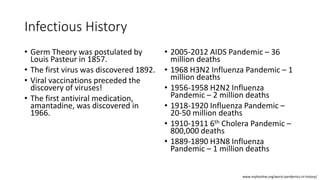
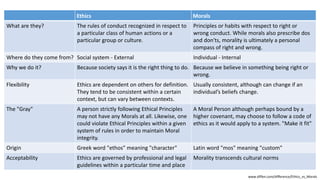
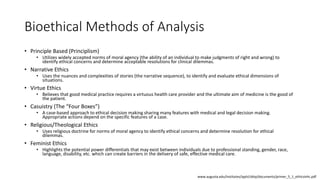
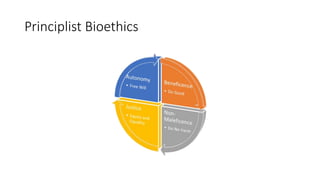
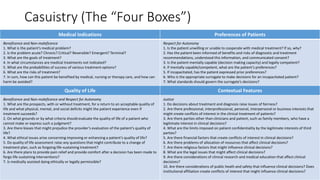
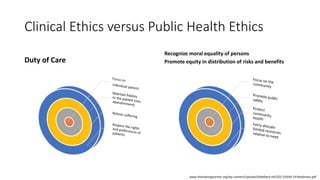
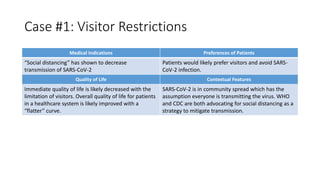
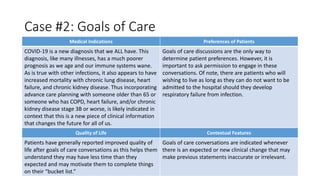
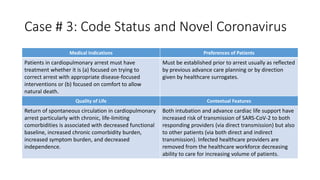
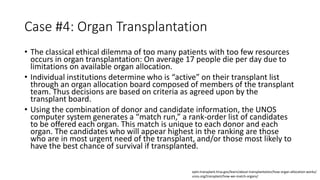
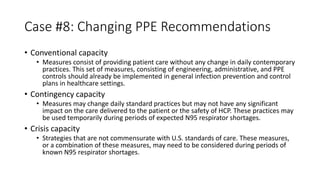
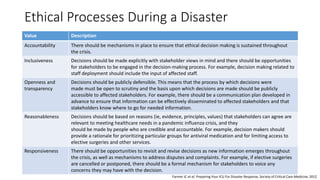
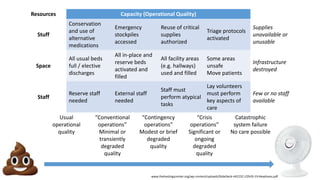
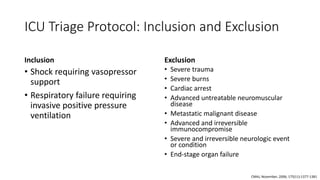
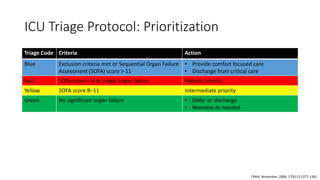
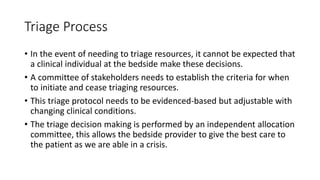
The document discusses ethics considerations during pandemics and public health emergencies. It begins with a brief history of pandemics and infectious diseases. It then covers various bioethical frameworks and methods of analysis that can be applied to challenges that arise, including principlism, narrative ethics, and casuistry. The document also discusses the differences between clinical ethics and public health ethics. It uses several case examples to demonstrate how different bioethical approaches could be applied to issues like visitor restrictions, goals of care conversations, changing PPE recommendations, and resource allocation. Throughout, it emphasizes the importance of transparency, inclusion, reasonableness and revisiting decisions as more information becomes available.