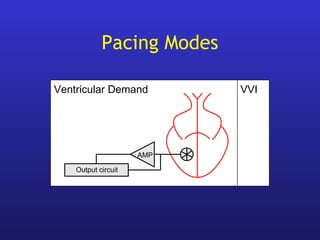
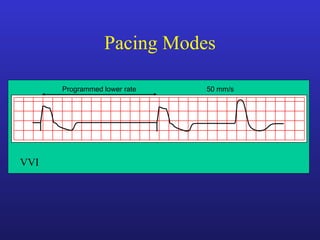
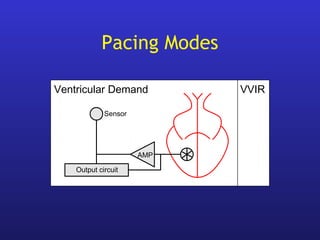
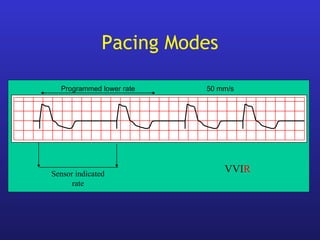
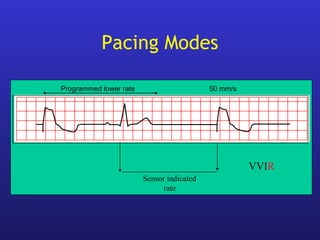
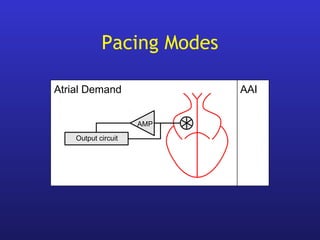
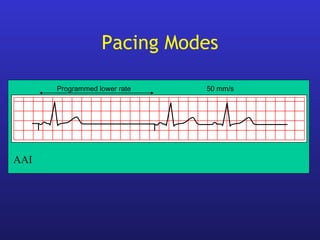
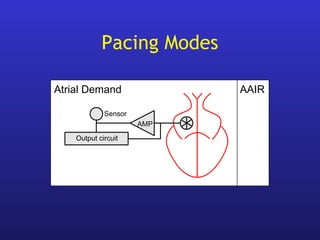
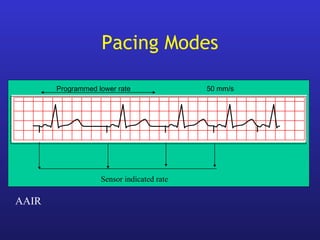
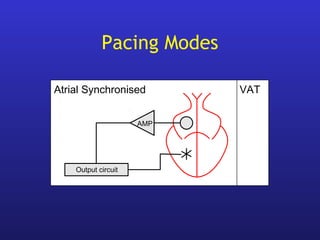
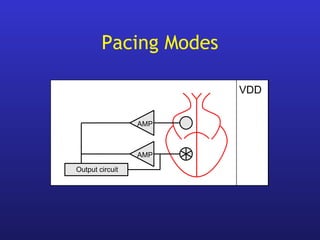
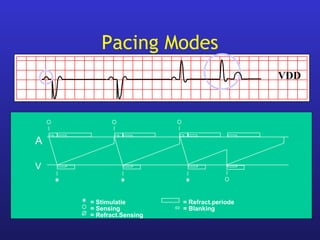
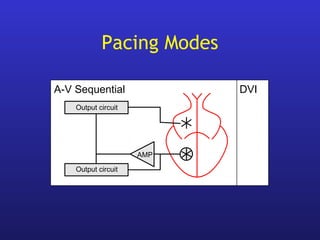
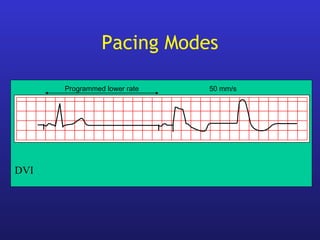
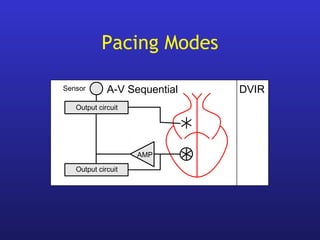
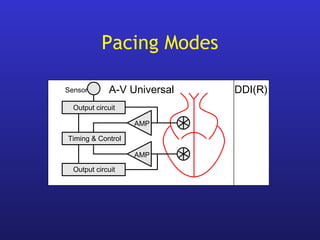
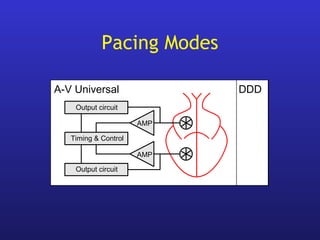
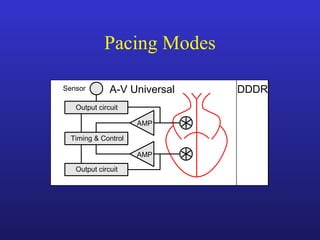
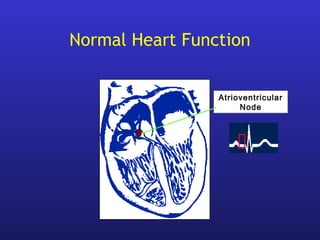
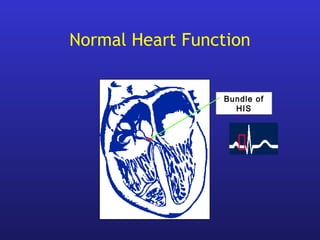
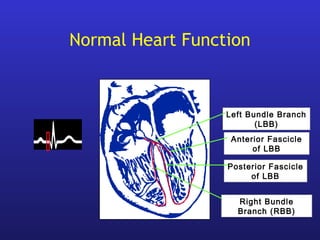
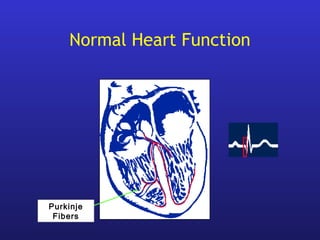
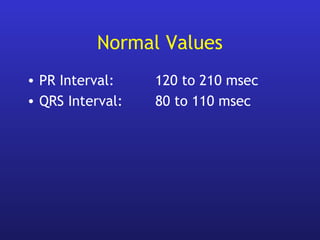
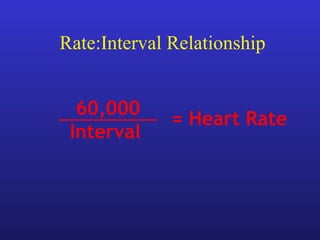
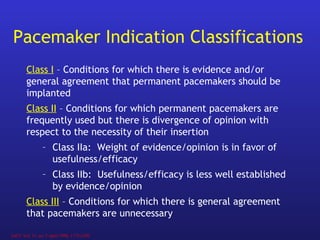
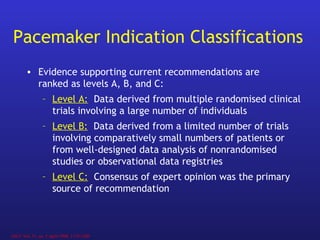
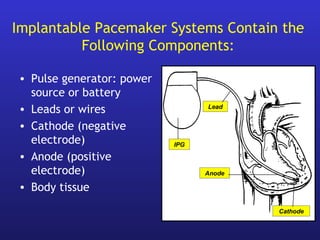
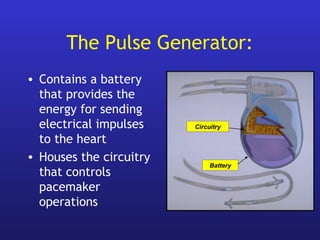
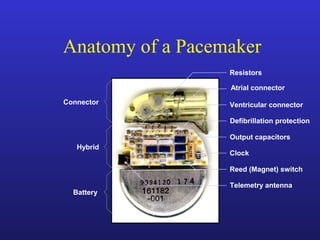
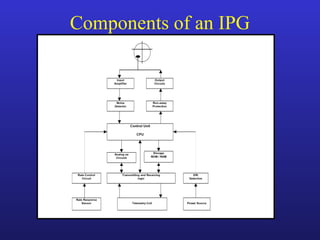
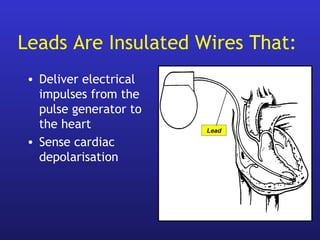
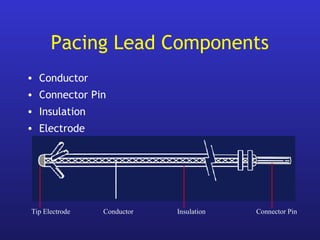
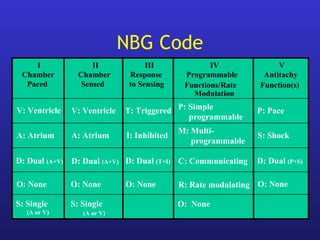
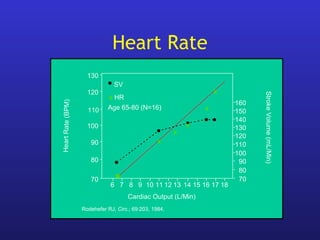
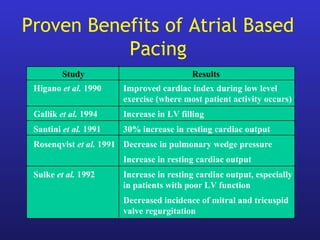
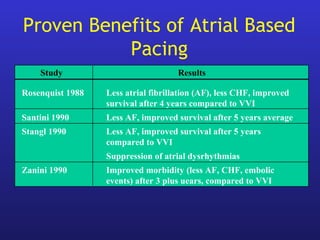
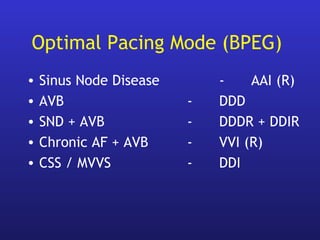
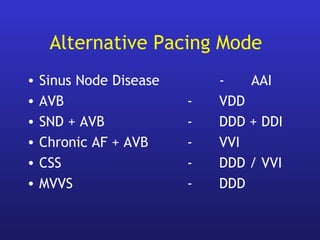
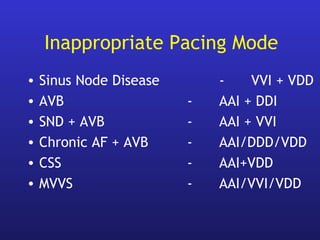
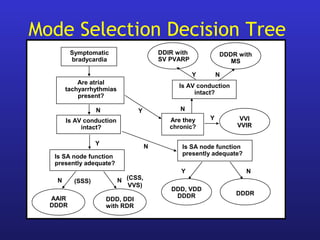
This document provides an overview of pacemakers, including their indications, components, and modes of operation. It discusses the types of heart block that qualify as indications for pacemaker implantation. The components of a pacemaker system include the pulse generator which contains the battery and circuitry, and leads which deliver electrical impulses from the generator to the heart and sense cardiac activity. Pacemakers operate in different modes defined by which chambers they pace and sense from. Choosing the optimal pacing mode aims to increase heart rate, maximize stroke volume, use atrial-based pacing, and maintain normal ventricular activation sequence.
![Summary of Pacemaker Indications
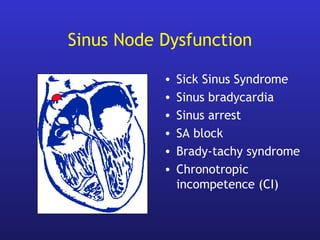
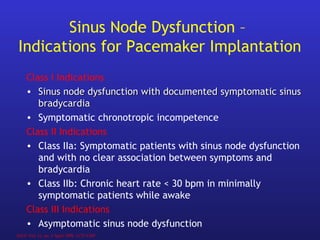
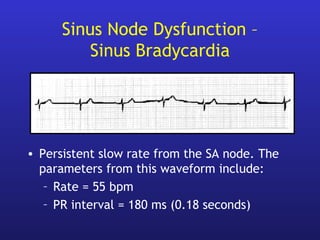
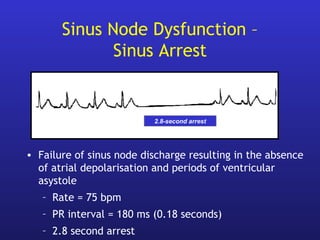
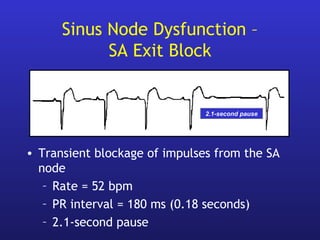
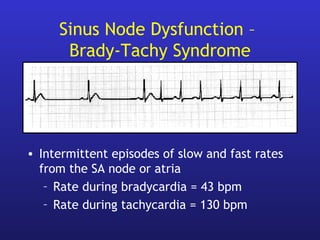
• Sinus node dysfunction
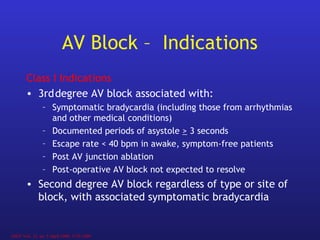
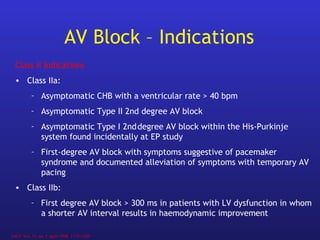
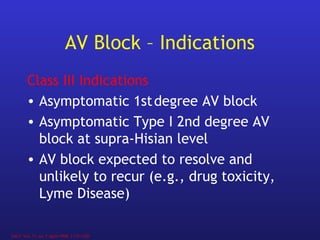
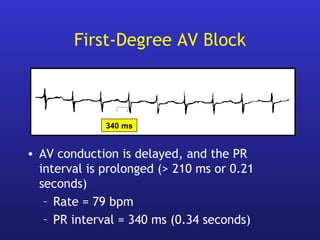
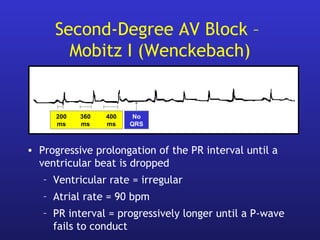
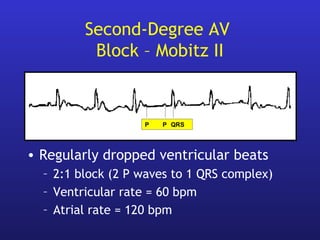
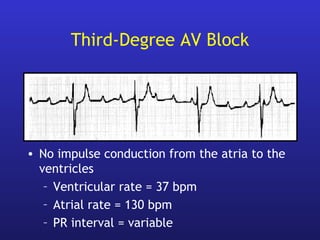
• AV block (Congenital, acquired, surgical)
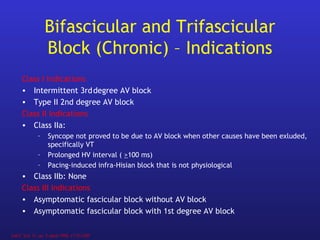
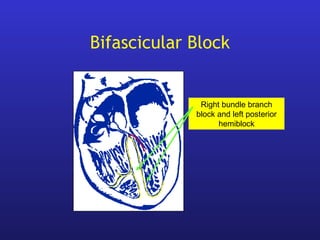
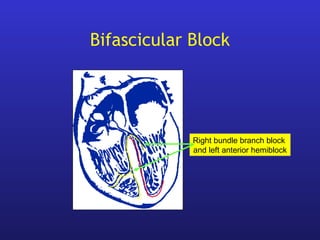
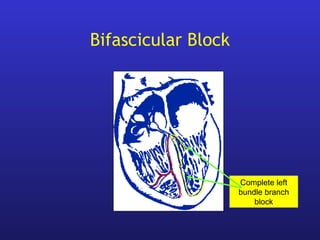
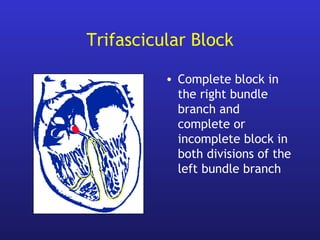
• Bifascicular and trifascicular block
• Hypersensitive Carotid Sinus Syndrome (CSS)
• [ Malignant Vasovagal Syncope (MVVS) ]
• Pacing after cardiac transplantation
• Heart Failure / HOCM / AF
• ( AHA/ACC and BPEG indications )](https://image.slidesharecdn.com/pacemakeroverview-180209135913/85/Pacemaker-overview-71-320.jpg)