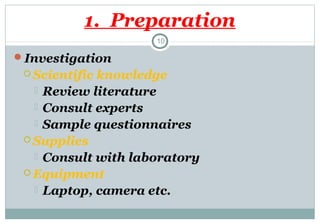
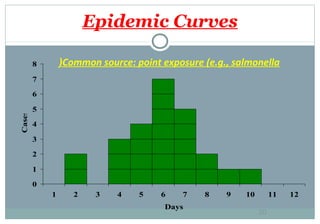
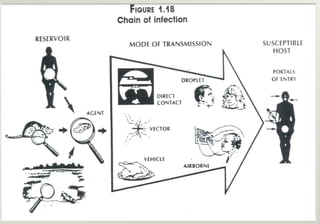
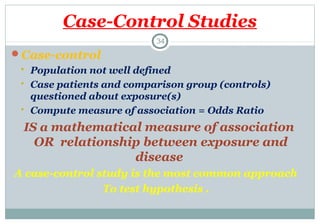
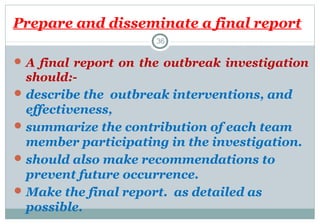
The document outlines guidelines for managing healthcare-associated infection (HAIs) outbreaks, emphasizing early detection and investigation to mitigate transmission among patients. It details steps for outbreak investigation, including verifying diagnoses, characterizing cases, and implementing control measures, while assigning roles and responsibilities to involved personnel. A thorough final report is essential to summarize the findings and recommendations to prevent future occurrences.