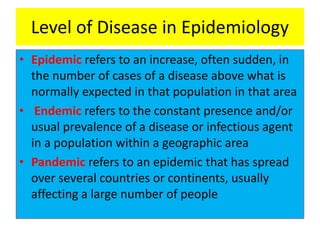
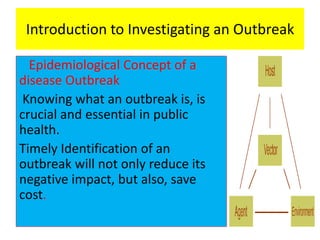
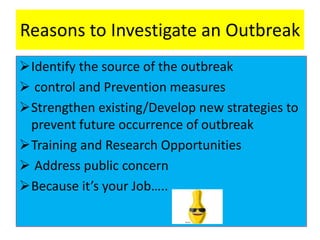
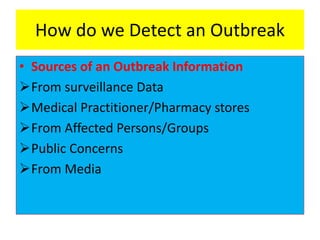
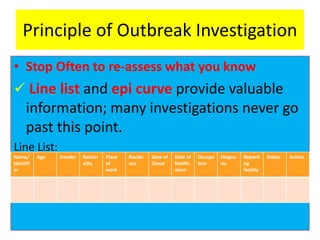
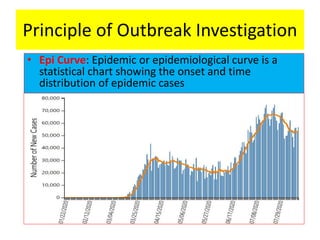
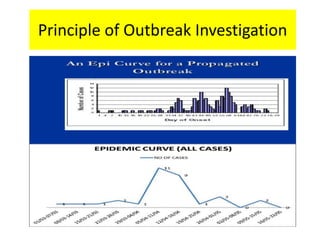
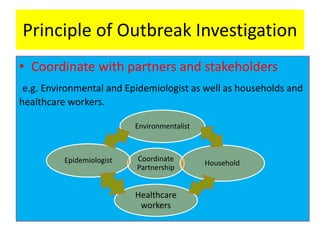
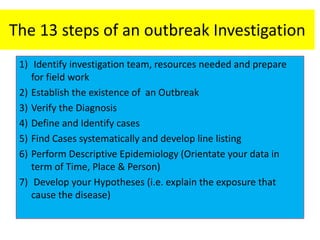
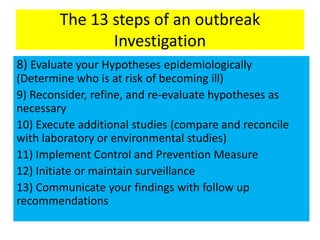
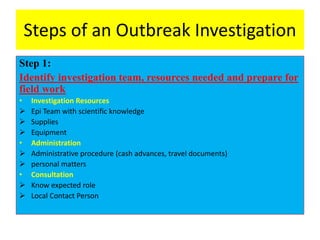
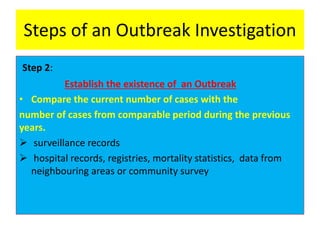
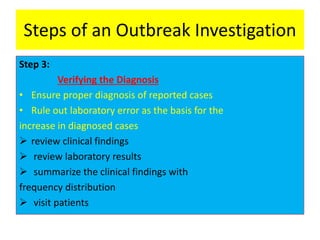
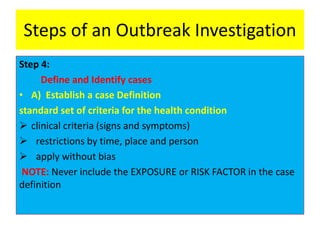
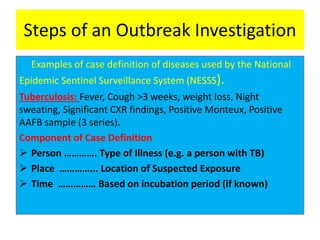
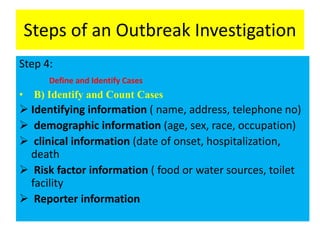
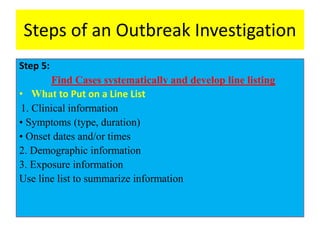
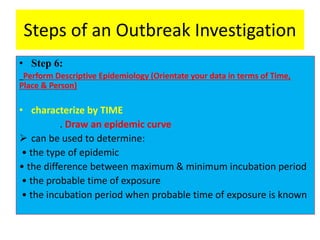
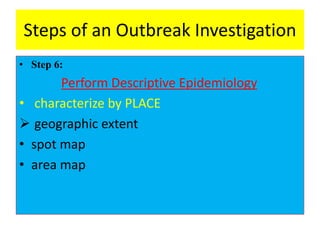
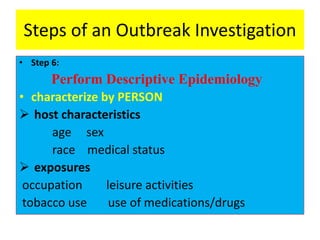
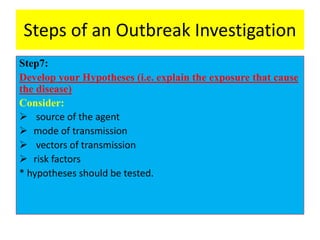
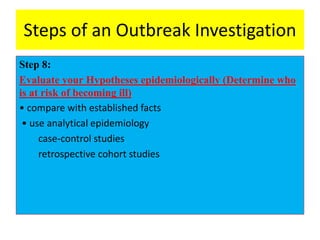
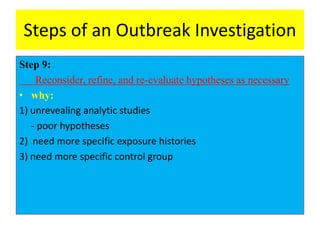
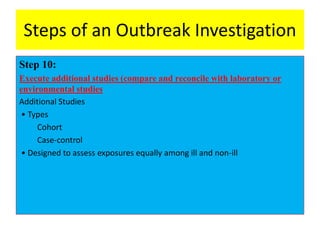
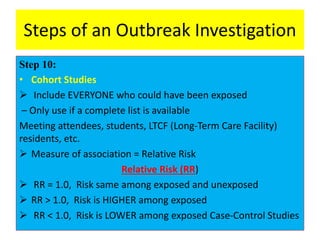
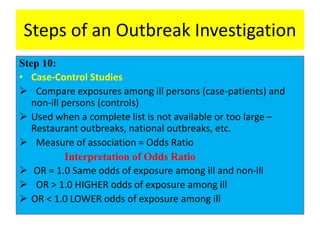
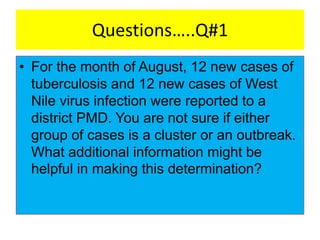
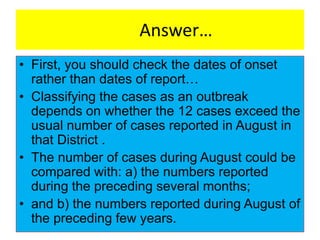
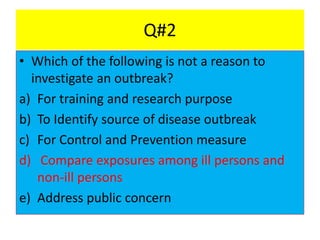
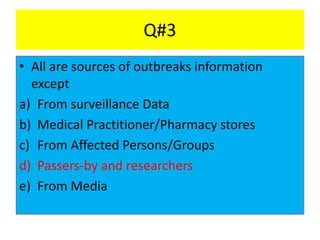
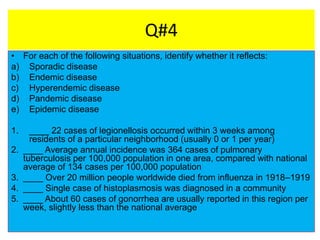
The document provides an overview of investigating disease outbreaks through a 13-step approach. It defines key epidemiological concepts like outbreak, epidemic, endemic and pandemic. The 13 steps include: 1) forming an investigation team, 2) verifying the existence of an outbreak, 3) verifying diagnoses, 4) defining cases, 5) finding cases systematically, 6) descriptive epidemiology, 7) developing hypotheses, 8) evaluating hypotheses, 9) refining hypotheses, 10) additional studies, 11) control measures, 12) surveillance, and 13) communication. Descriptive epidemiology involves characterizing cases by time, place and person. Hypothesis development and evaluation use epidemiological and analytical methods.