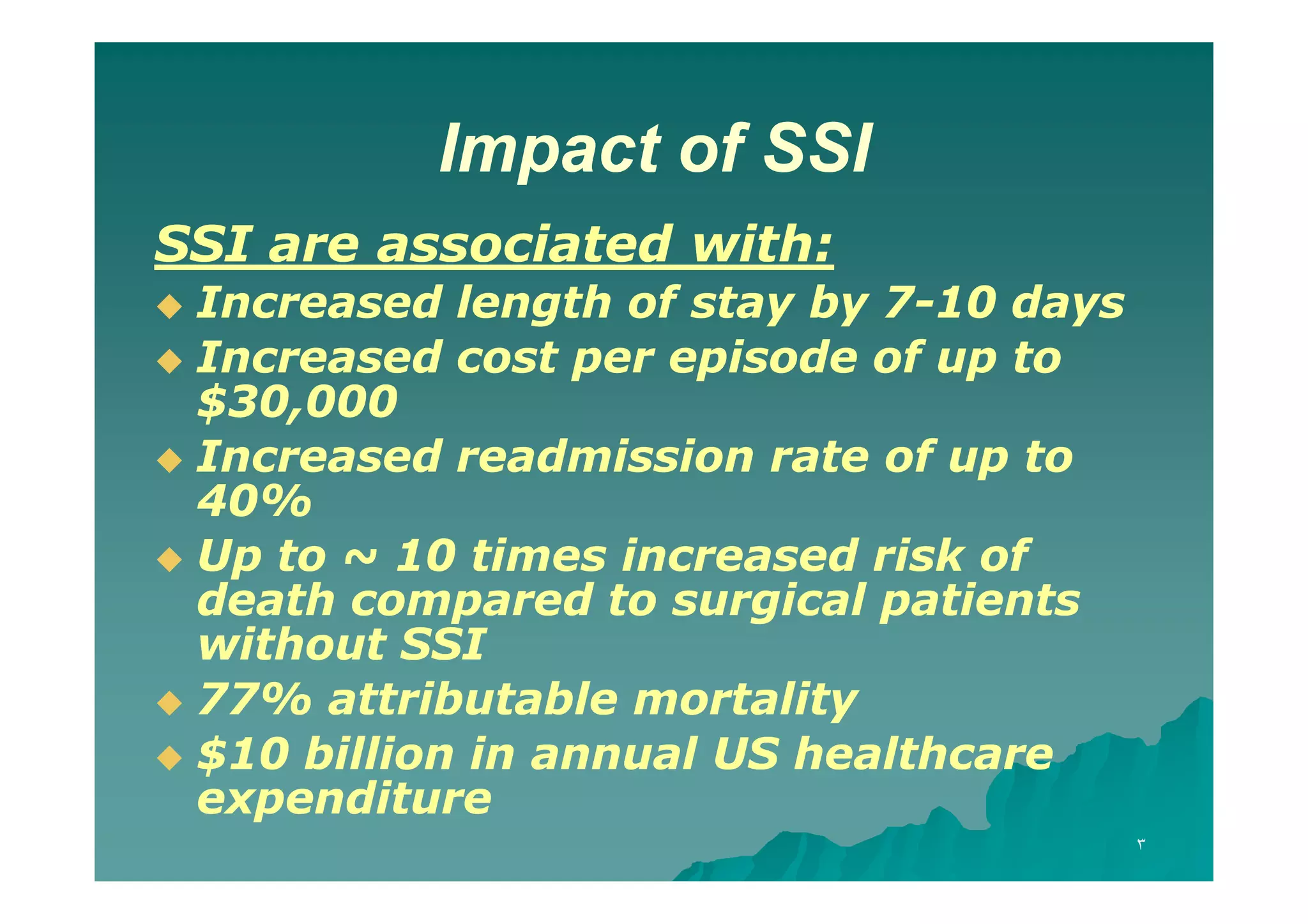
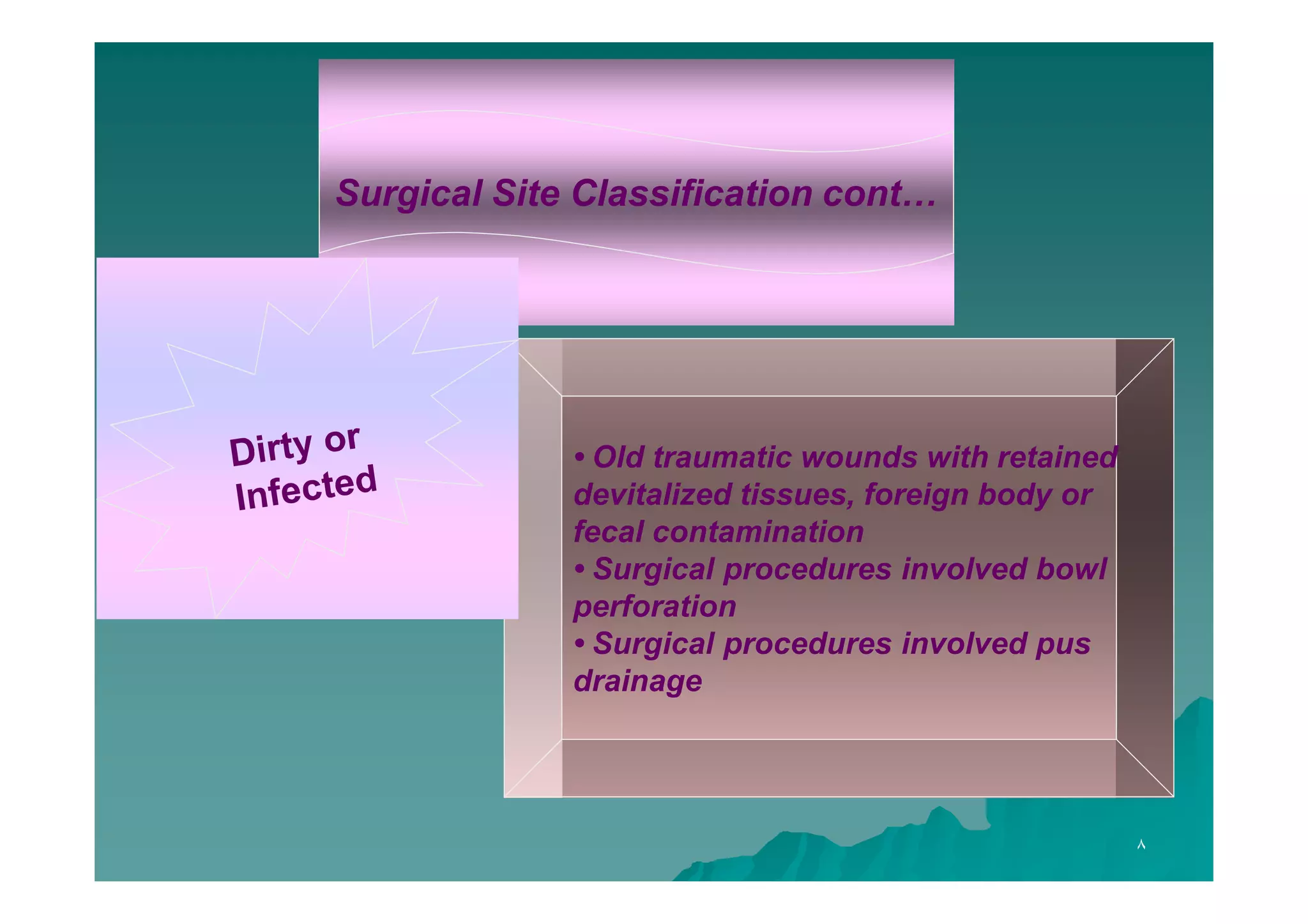
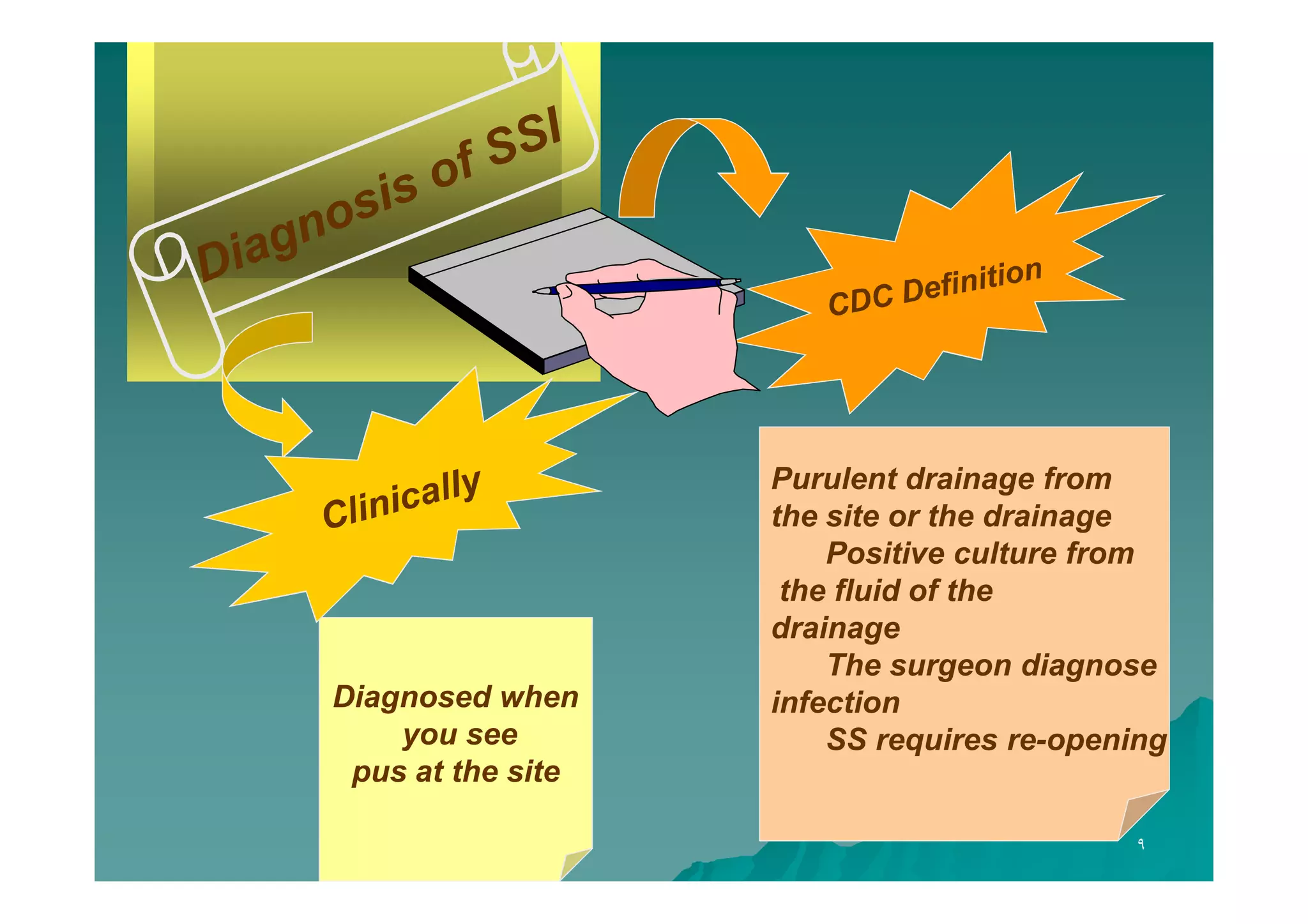
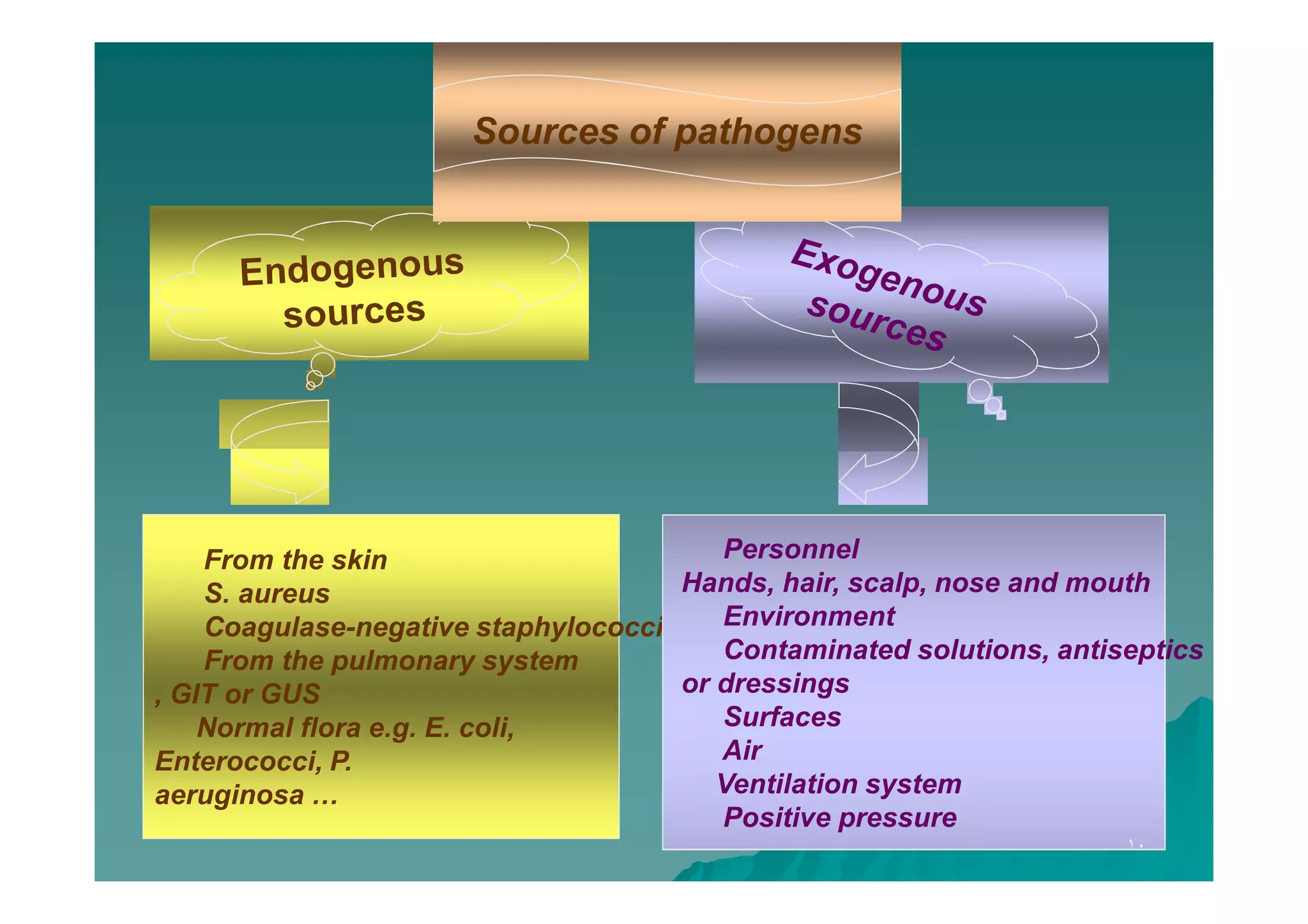
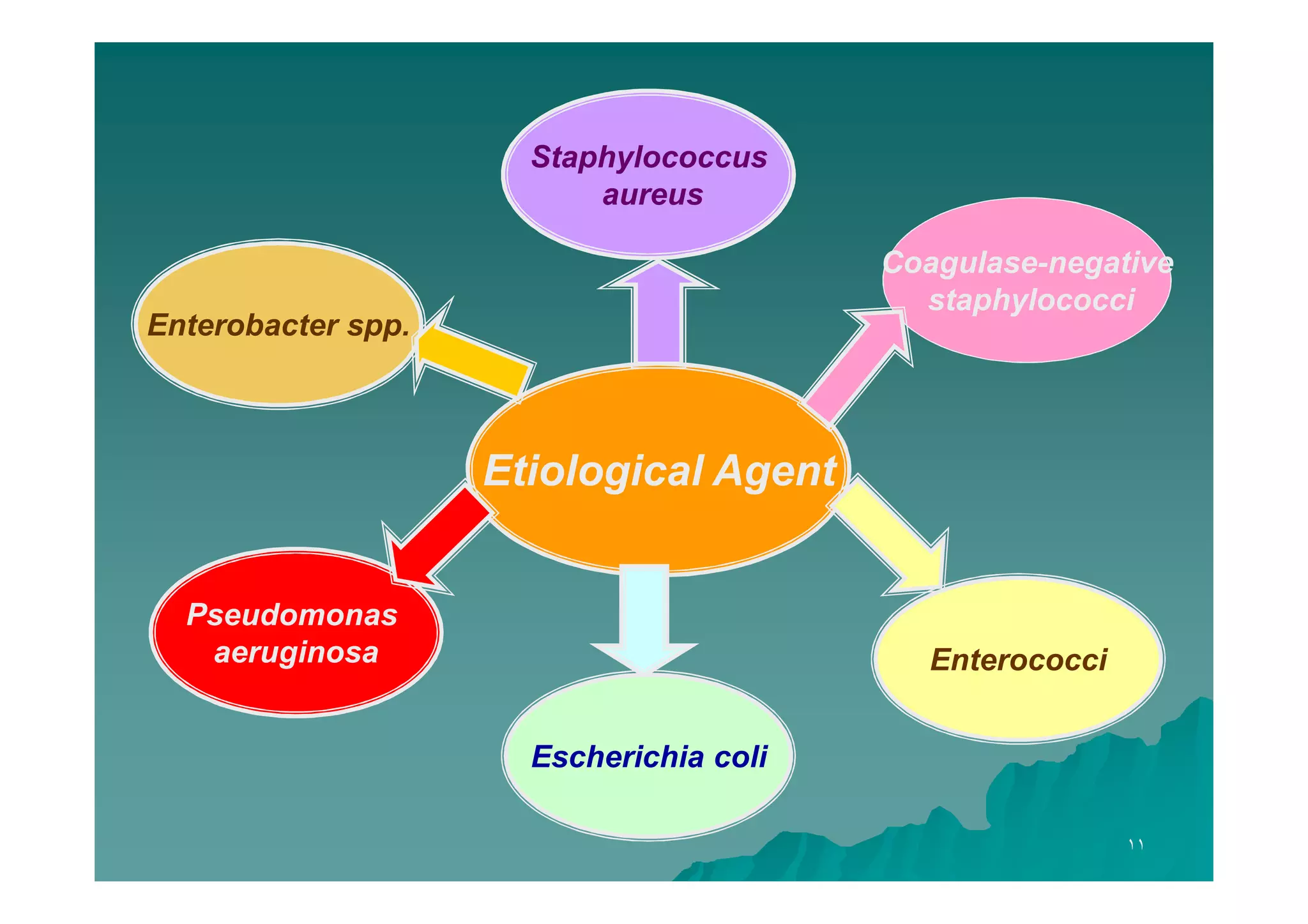
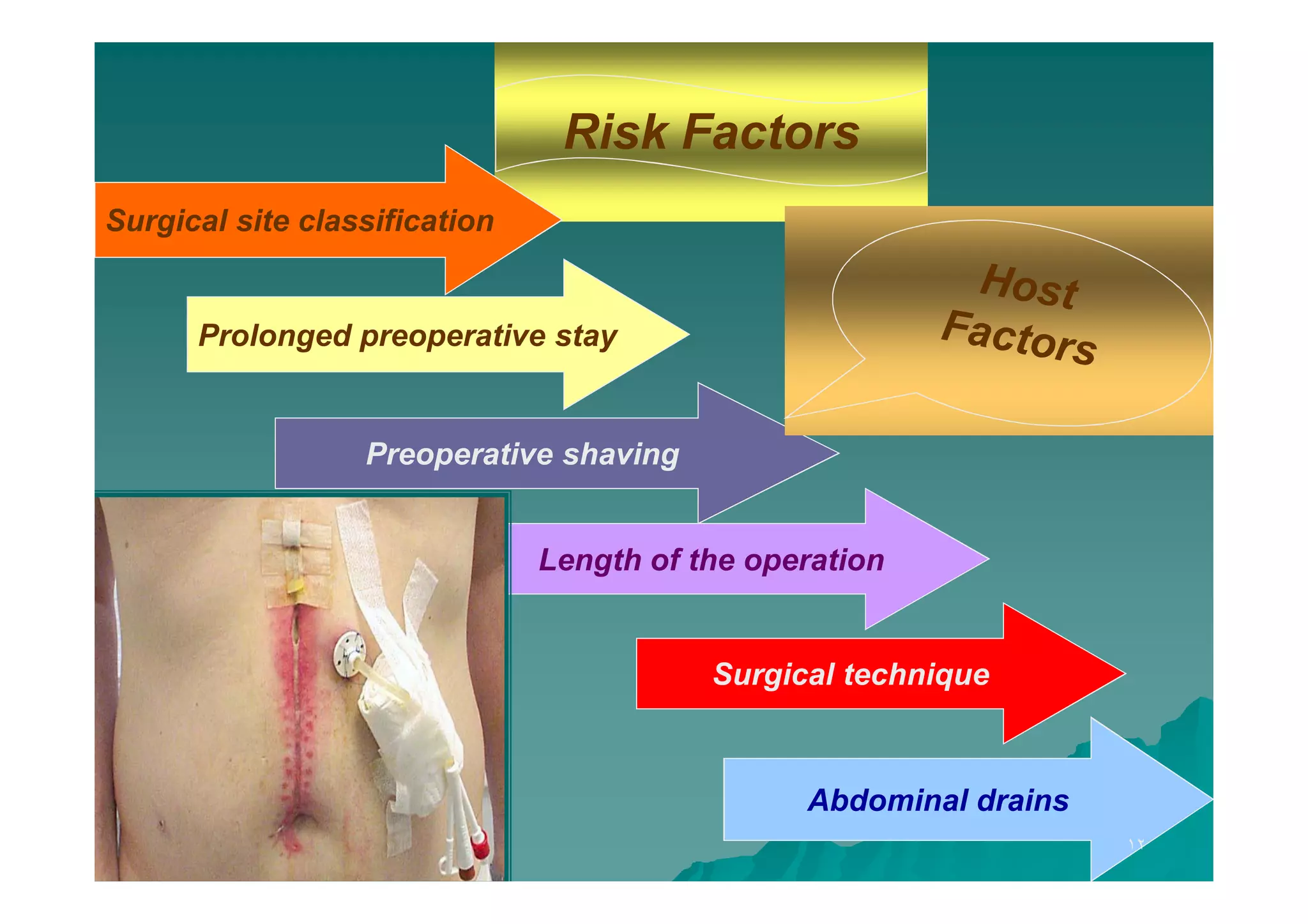
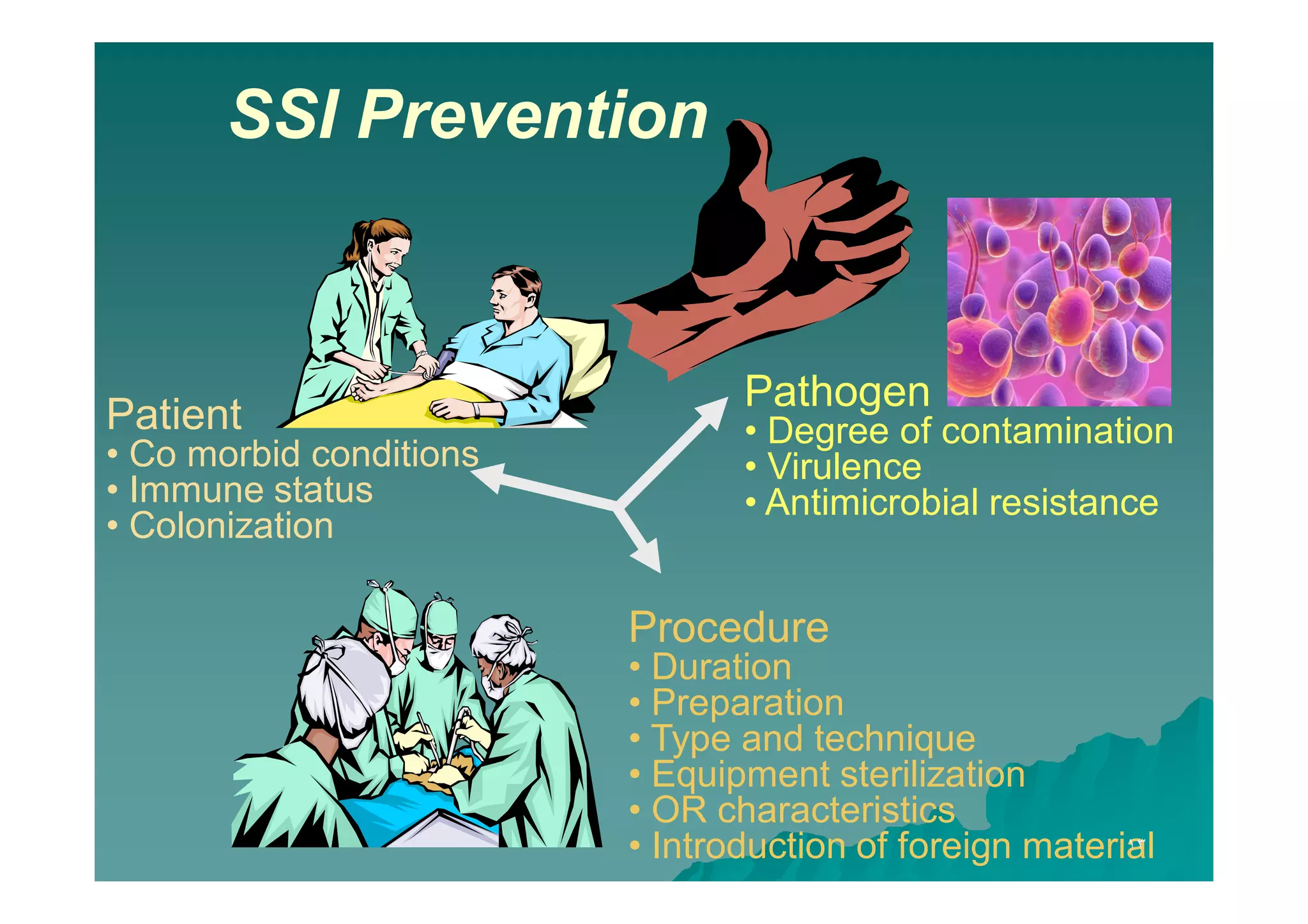
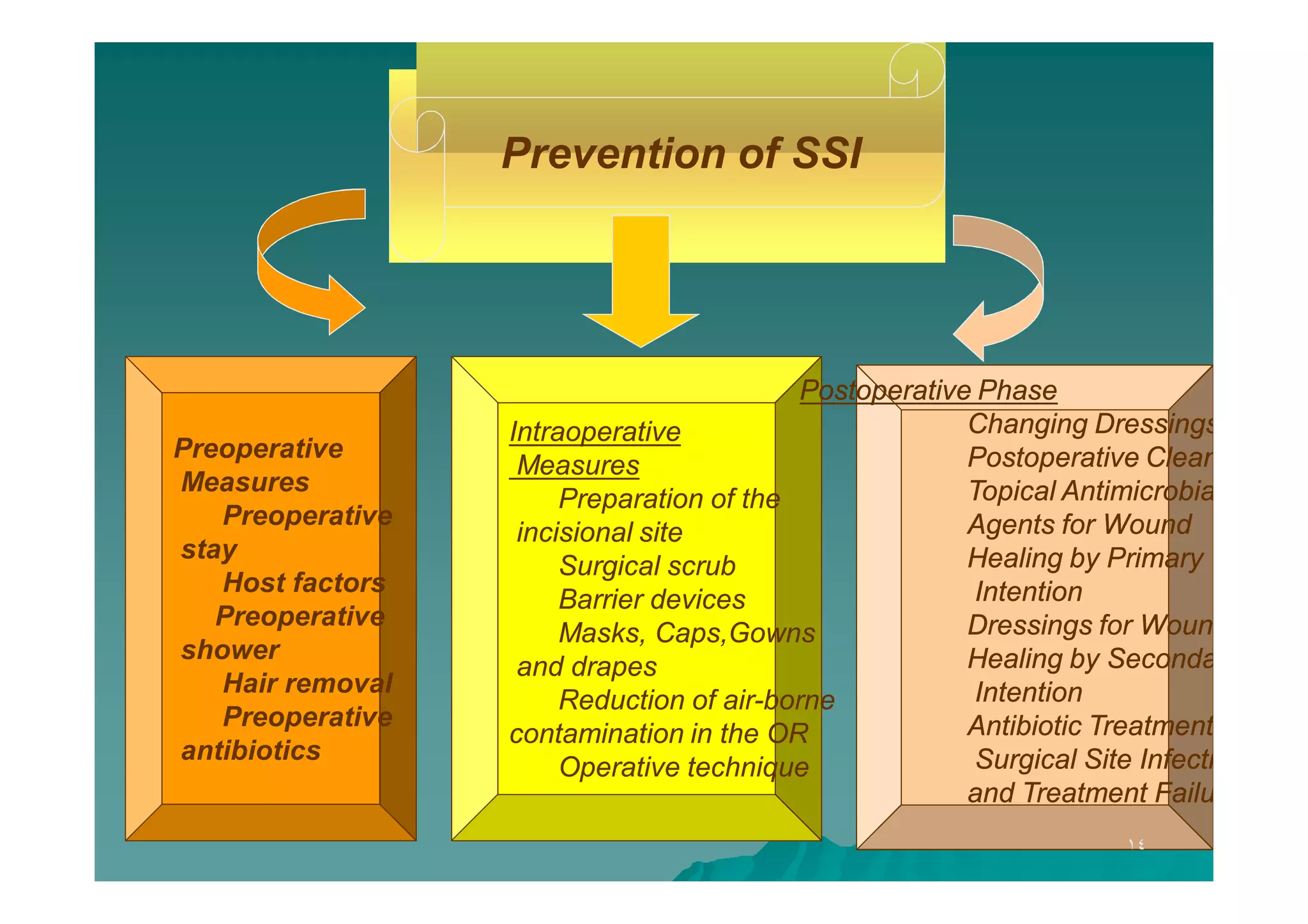
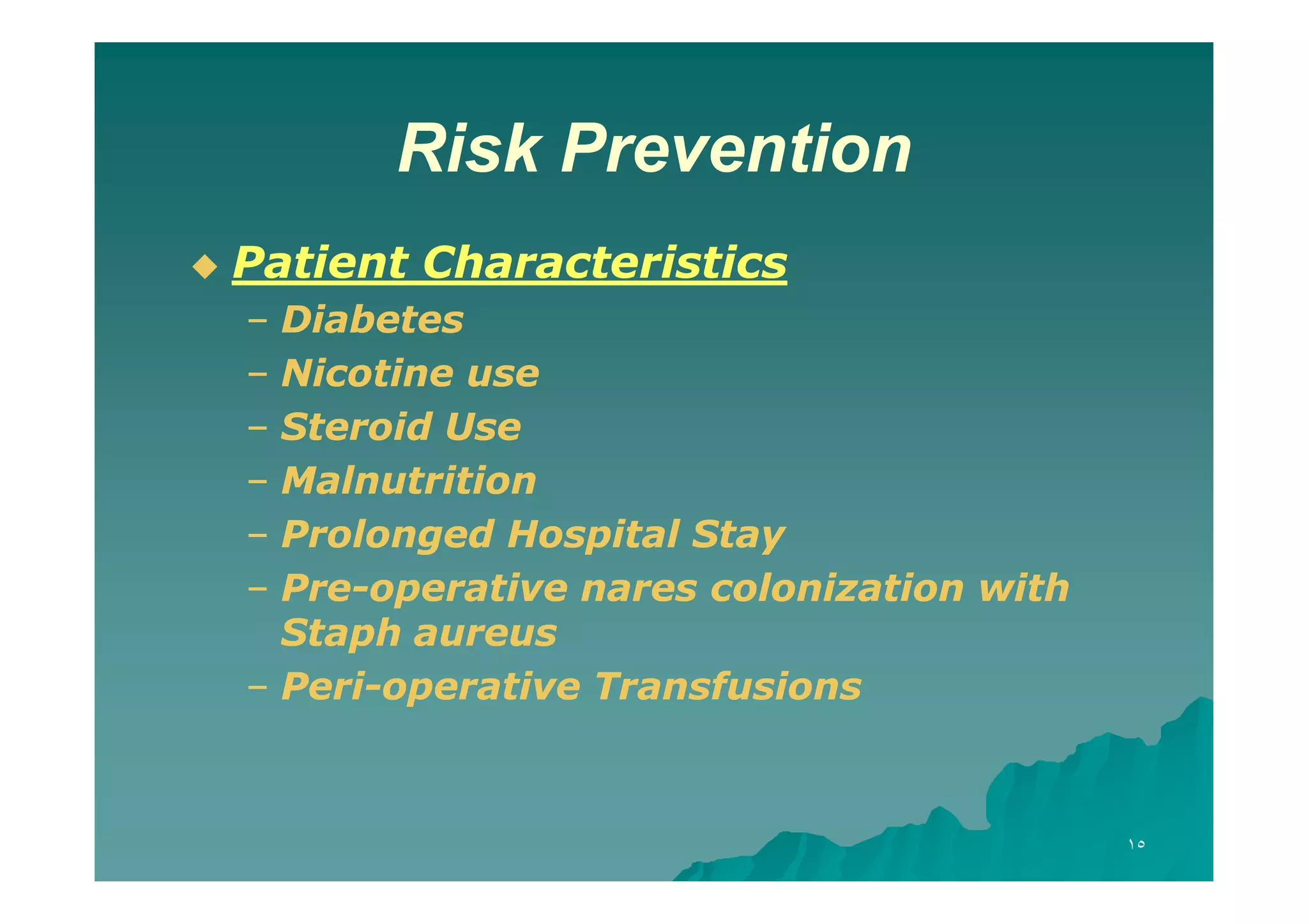
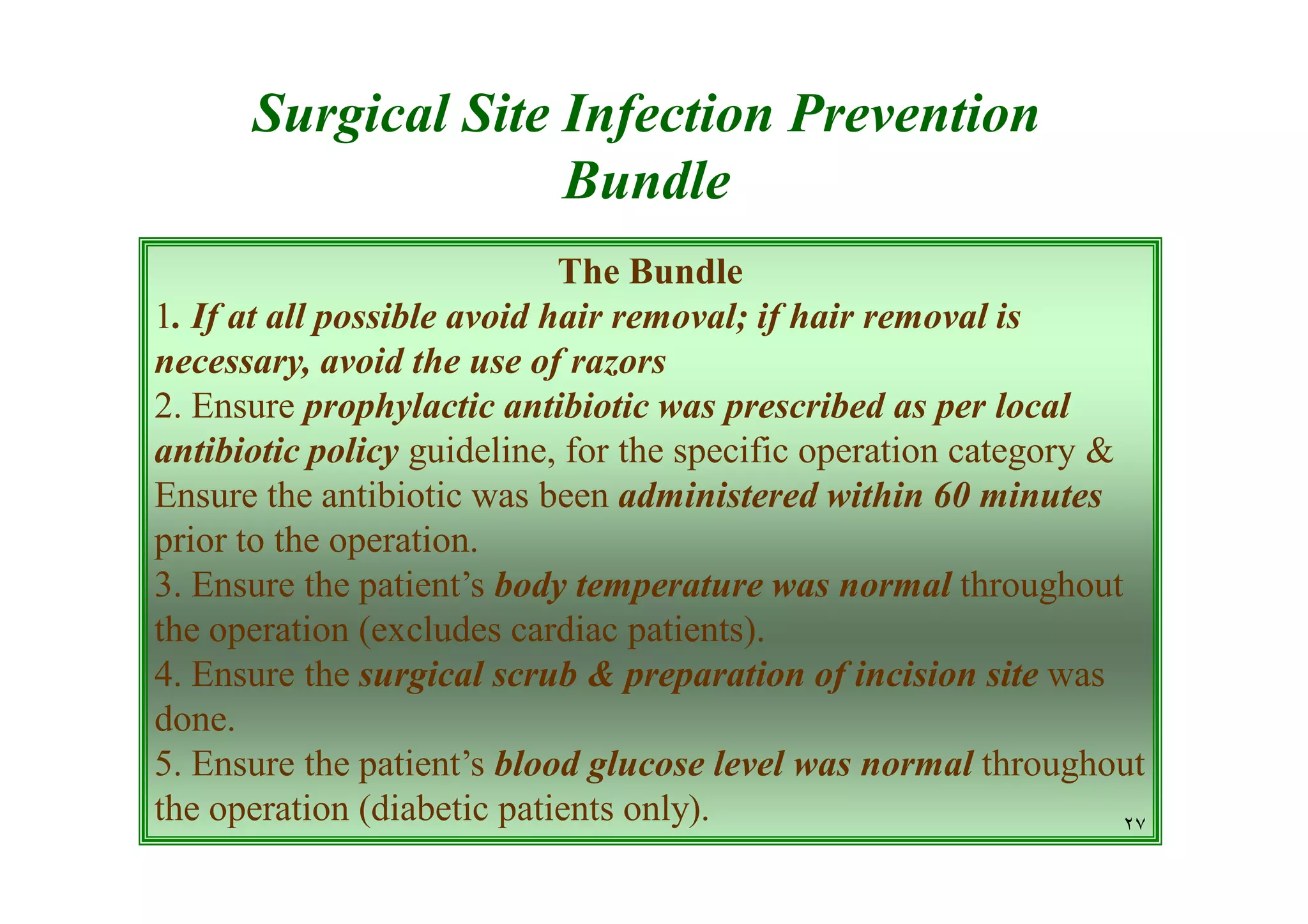
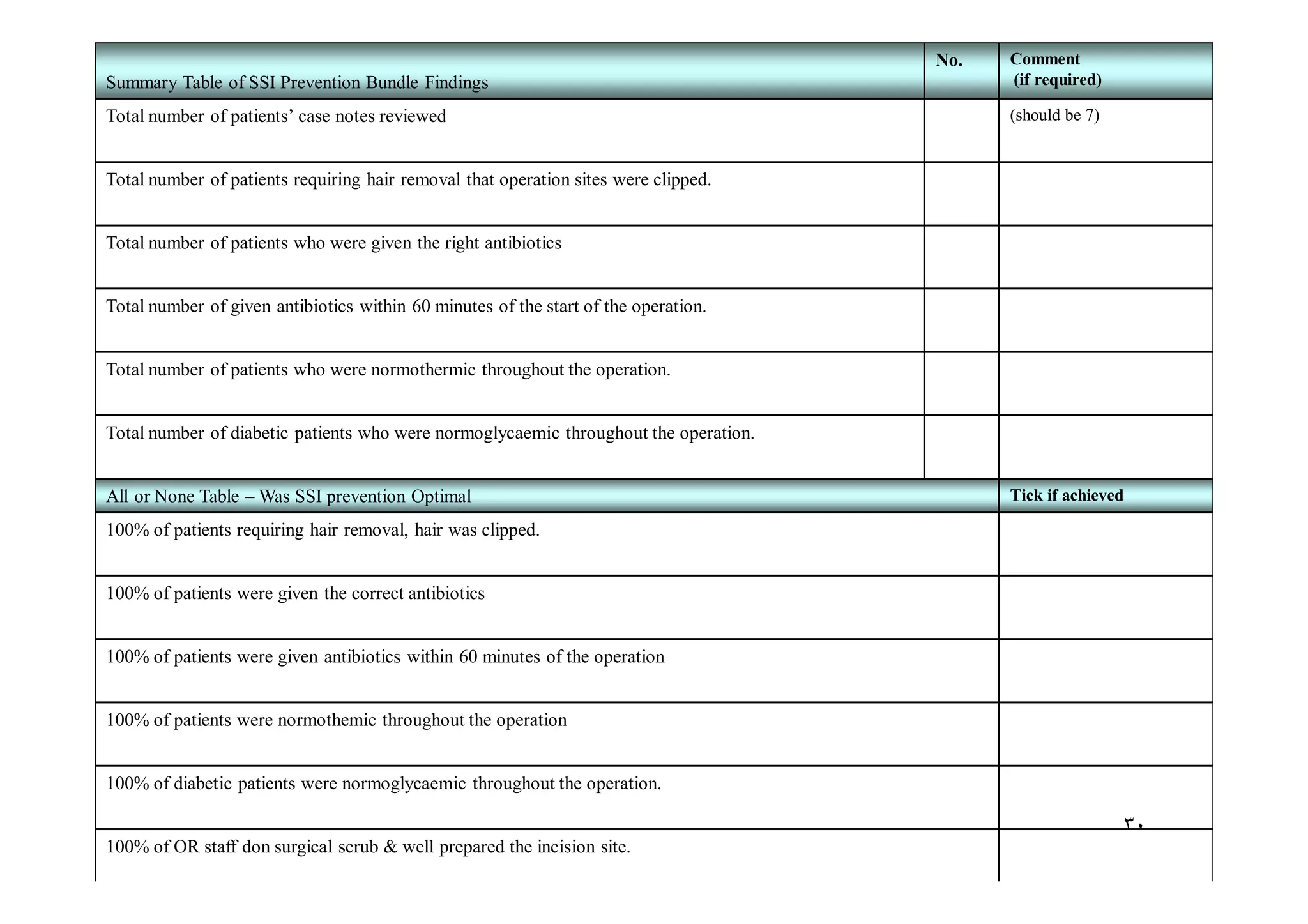
The document discusses the prevalence and impact of surgical site infections (SSI), highlighting their association with increased patient morbidity, mortality, and healthcare costs. It outlines SSI classifications, risk factors, and prevention strategies, emphasizing the importance of proper hygiene, surgical techniques, and antibiotic use before and after surgery. Additionally, it introduces an SSI prevention bundle aimed at optimizing peri-operative care to minimize infection risks and improve patient outcomes.