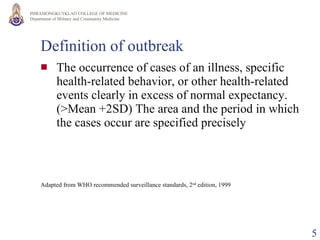
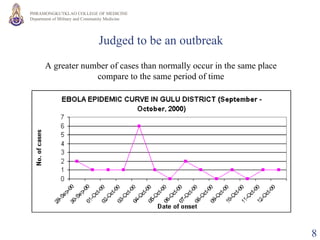
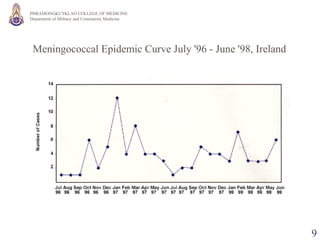
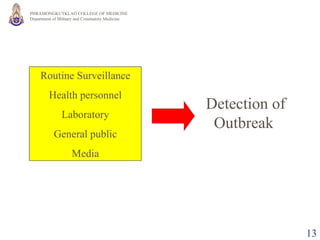
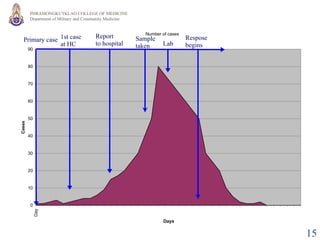
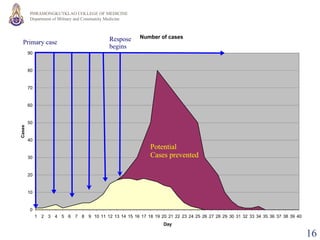
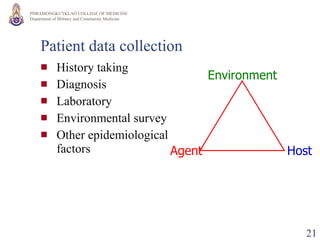
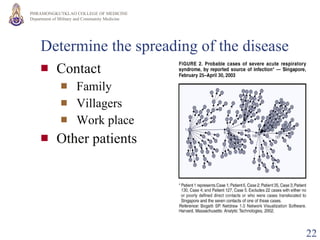
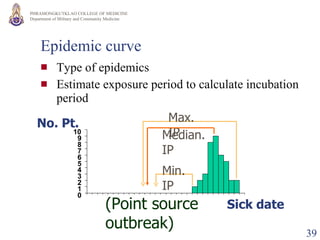
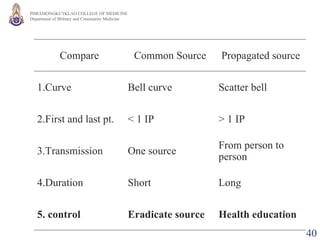
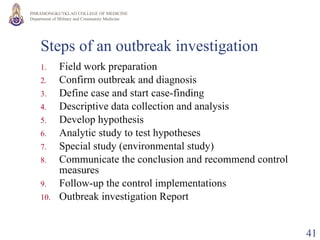
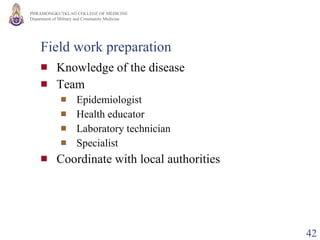
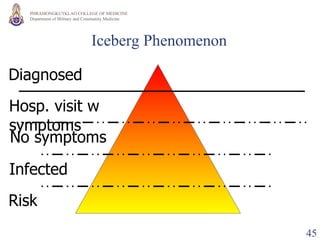
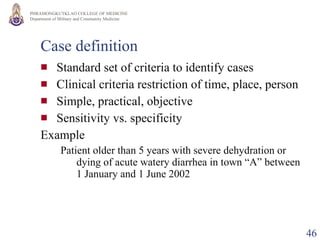
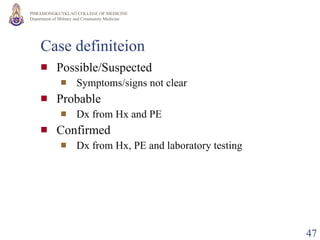
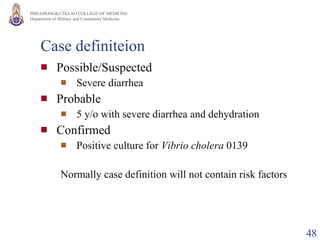
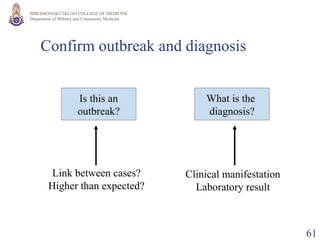
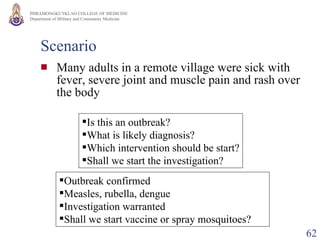
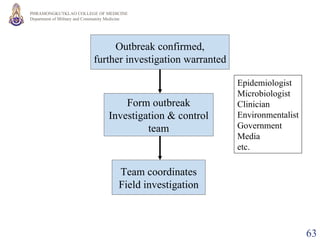
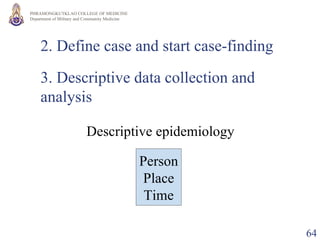
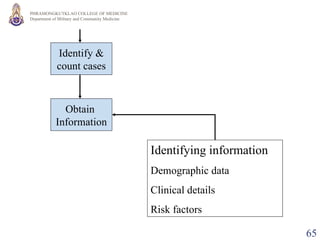
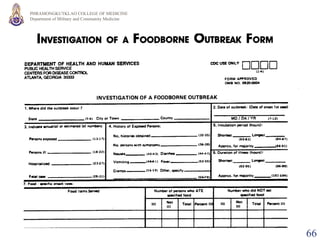
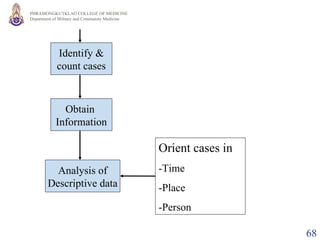
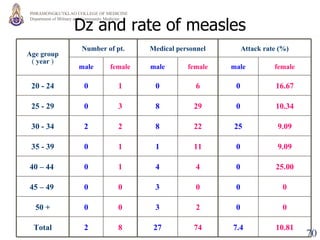
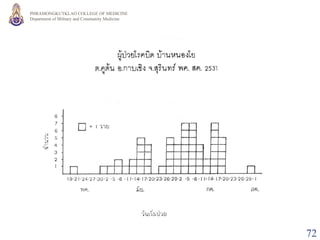
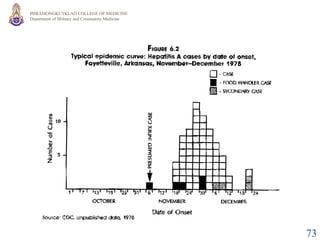
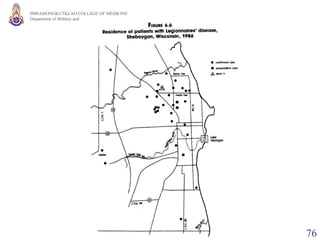
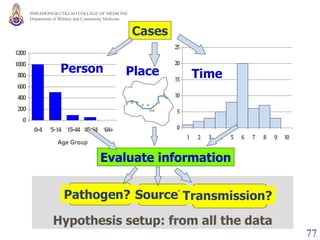
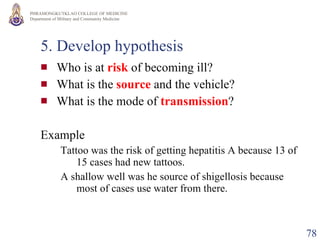
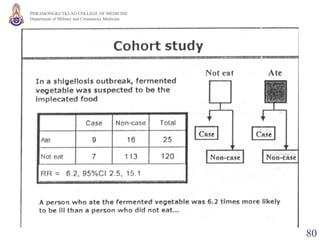
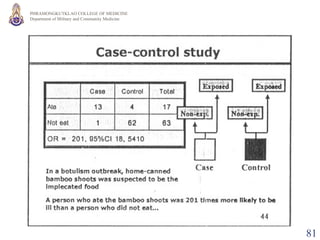
The document outlines the key principles and steps of conducting an outbreak investigation. It defines what constitutes an outbreak and explains that the purpose is to control the current outbreak, prevent future occurrences, and evaluate existing surveillance and prevention programs. The main steps described are confirming the outbreak, defining cases, collecting descriptive data, developing hypotheses, testing hypotheses through analytical studies, communicating conclusions, and recommending control measures.