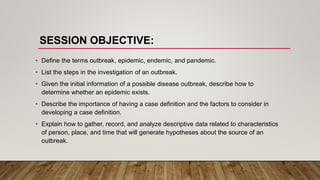
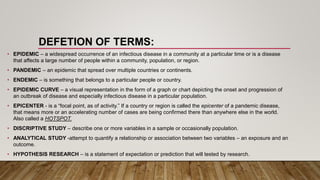
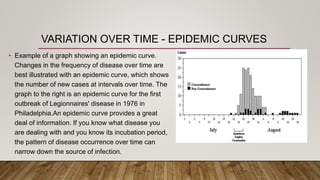
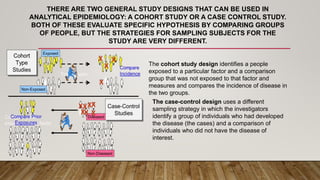
The document outlines the procedures and significance of investigating virus outbreaks in the 21st century, detailing the definitions of key terms such as epidemic, pandemic, and endemic. It describes the systematic steps involved in outbreak investigation, including case definition, data collection, hypothesis development, and the implementation of control measures. Clear guidance is provided on the roles of health authorities, the use of descriptive and analytical epidemiology, and the importance of communicating findings effectively.