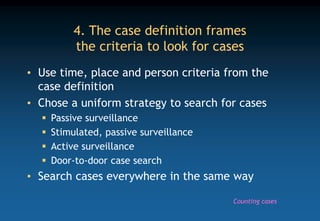
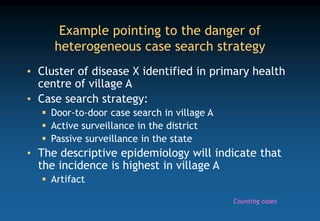
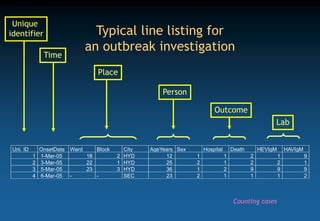
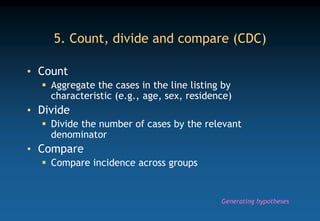
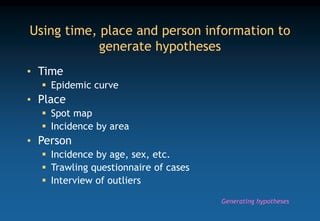
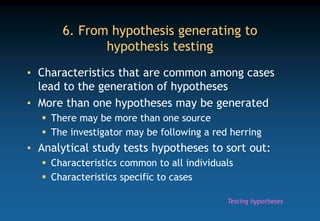
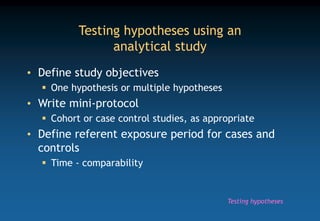
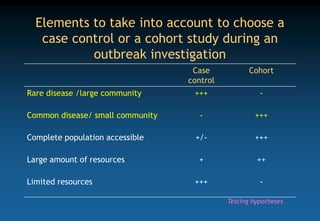
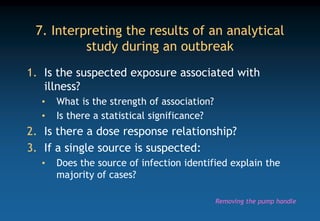
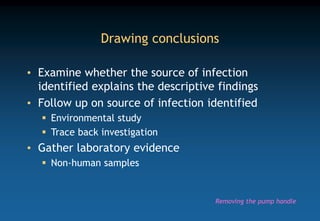
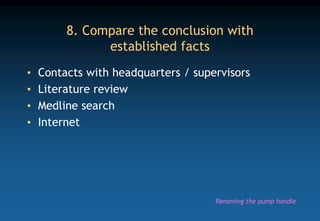
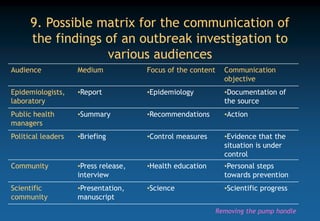
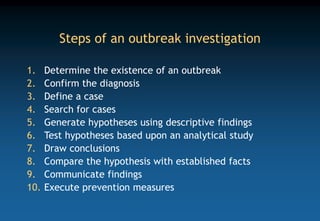
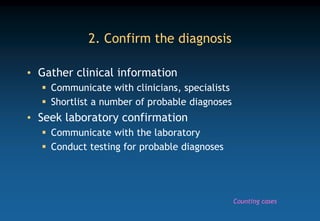
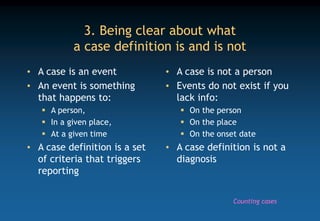
The document outlines the 10 steps of conducting an outbreak investigation: 1) determine existence of outbreak, 2) confirm diagnosis, 3) define cases, 4) search for cases, 5) generate hypotheses, 6) test hypotheses, 7) draw conclusions, 8) compare to facts, 9) communicate findings, and 10) execute prevention measures. Key steps include defining a case, systematically searching for cases, analyzing descriptive findings to generate hypotheses, testing hypotheses through analytical studies to identify the source, communicating conclusions, and implementing control measures to prevent future outbreaks.
![Prototype case definition
• A case is the occurrence of [spell out syndrome]
in a resident of [ spell out location] between
[beginning date] and [end date]
• Use of standardized syndromic case definition is
preferable
Integrated Disease Surveillance Programme
WHO
CDC
Counting cases](https://image.slidesharecdn.com/dha11outbreakinvestigation-231027141922-107c6bb3/85/DHA11_Outbreak-investigation-ppt-6-320.jpg)