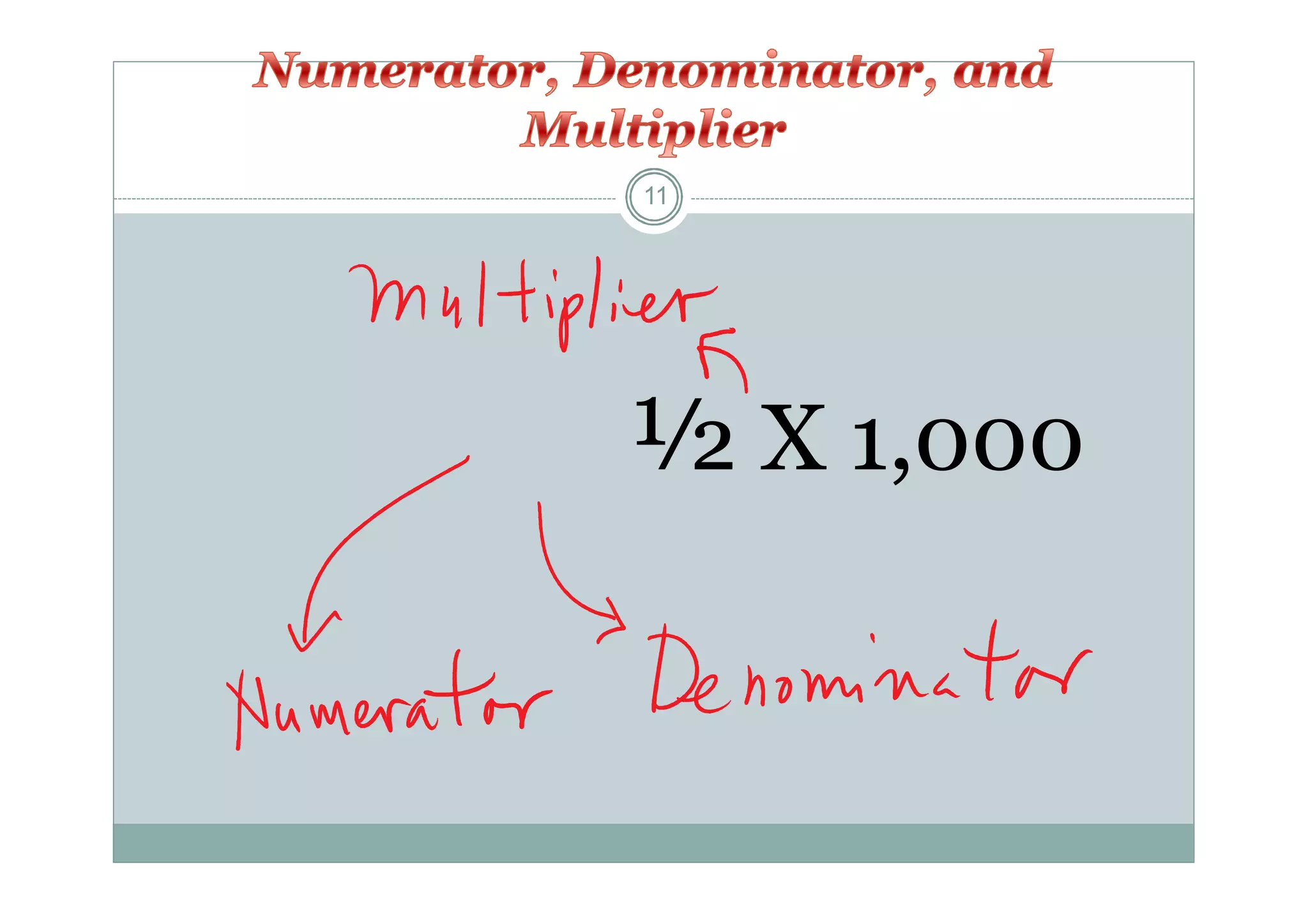
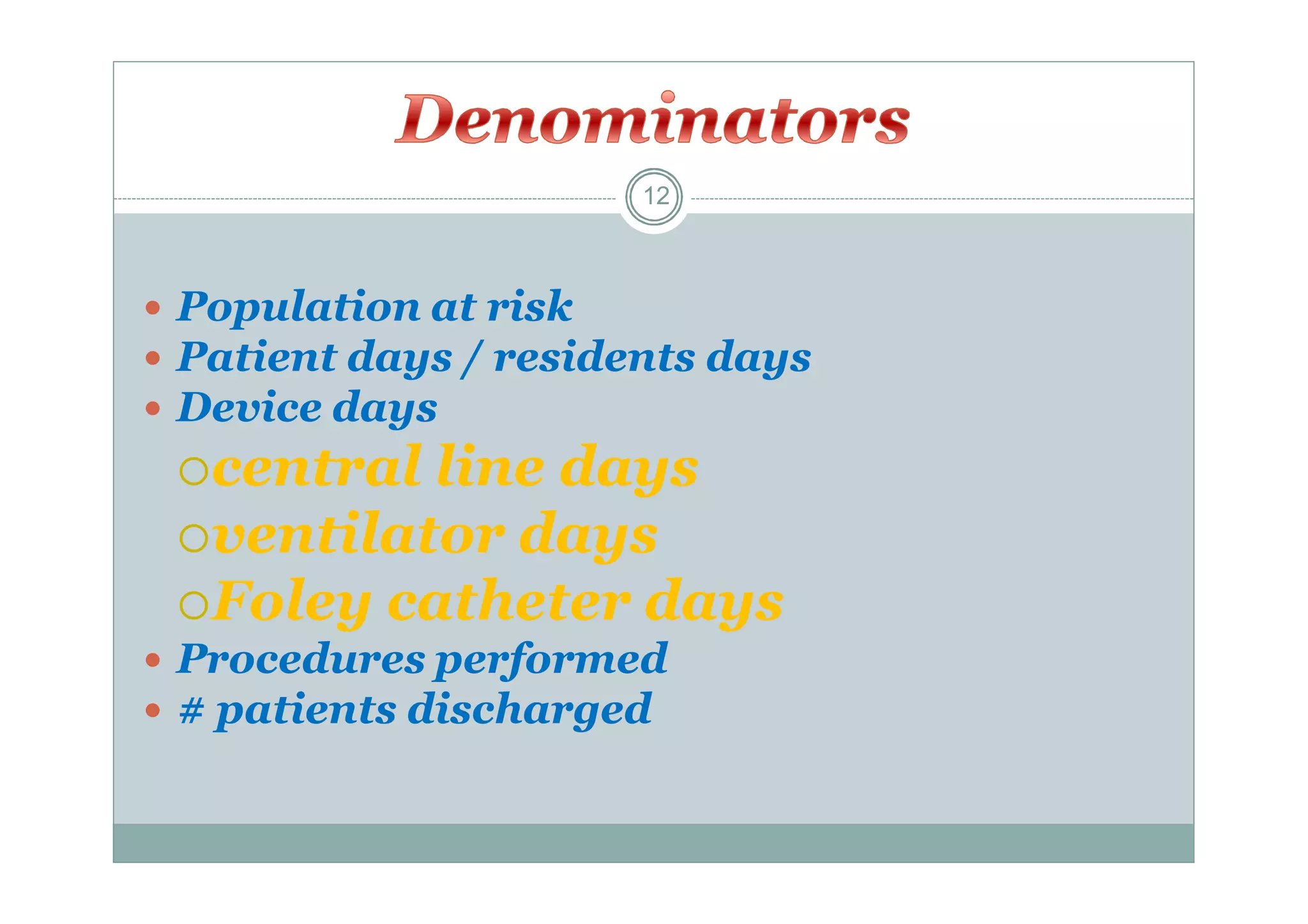
Surveillance involves the systematic and continuous collection and analysis of data for diseases or health conditions in a population. It can be active, involving proactive monitoring approaches, or passive, involving retrospective data review. Surveillance programs typically focus on specific infections, units, pathogens, or procedures based on risk assessments. The goals are to detect outbreaks early, identify prevention opportunities, and disseminate findings to improve health outcomes.