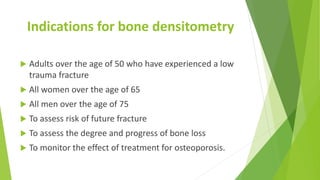
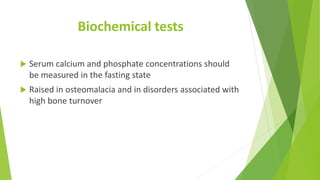
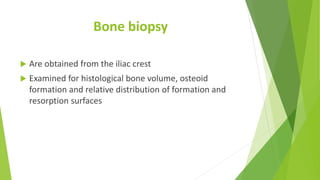
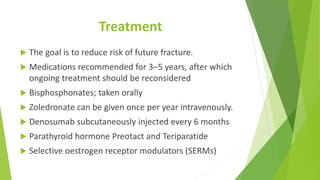
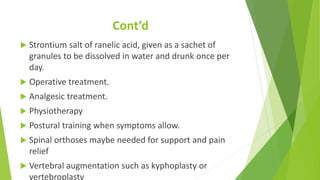
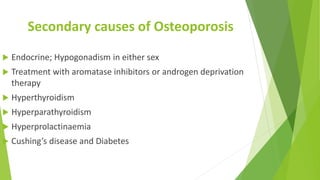
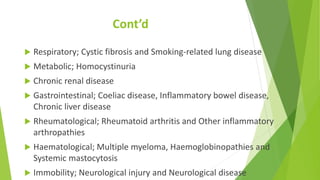
This document discusses metabolic and endocrine bone disorders like osteoporosis. It describes how these disorders may present as bone deformities in children, fractures in elderly patients, or bone pain and fractures in those taking corticosteroids. It covers examining patients, diagnostic tests like x-rays and bone density scans, biochemical tests, and bone biopsies. Risk factors, features, and treatments of postmenopausal osteoporosis are outlined, along with secondary causes of osteoporosis from endocrine, respiratory, metabolic, gastrointestinal, and other conditions. Prevention and treatment aim to reduce future fracture risk through medications or surgery.