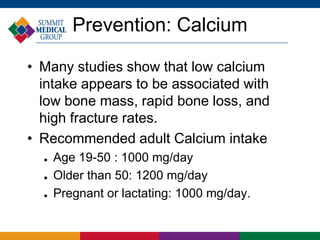
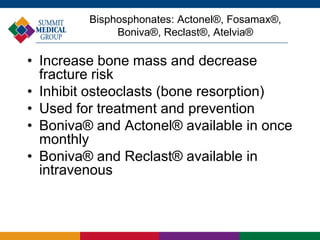
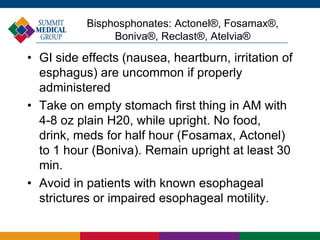
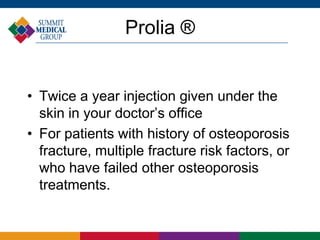
Osteoporosis is a condition characterized by decreased bone density due to an imbalance between bone resorption and formation, often referred to as the 'silent disease' because it presents without symptoms until fractures occur. Risk factors include age, gender, ethnicity, family history, and lifestyle choices such as diet and exercise, while prevention strategies focus on nutrition, exercise, and fall prevention. Diagnosis is typically conducted using a painless bone density measurement test, and treatment options vary based on individual risk factors and health status.