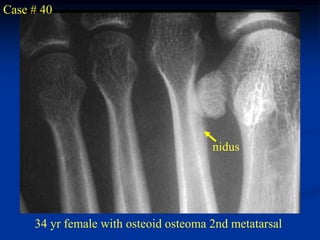
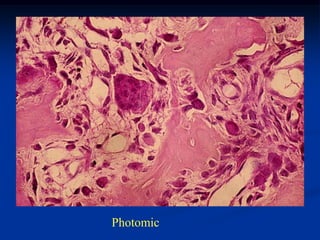
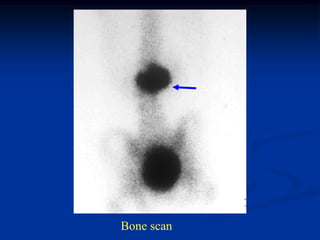
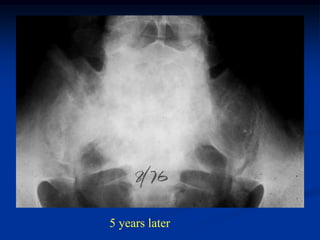
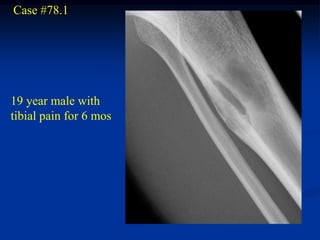
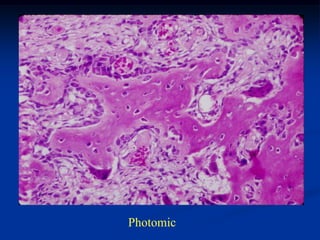
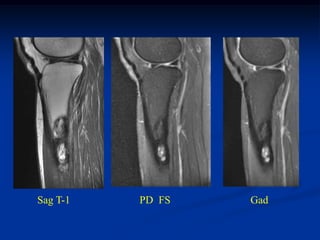
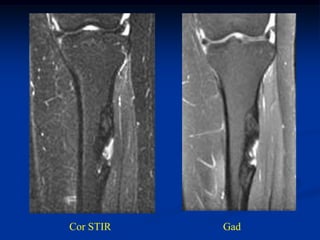
This document provides a summary of 50 cases of osteoid osteoma and osteoblastoma. Case 1-50 cover osteoid osteoma, with the classic presentation of a painful nidus most commonly in long bones that is diagnosed using imaging such as CT scan and bone scan. Case 51-94 cover osteoblastoma, a larger variant of osteoid osteoma that is treated surgically via curettage. The remainder of cases provide further examples and variations of these two conditions.