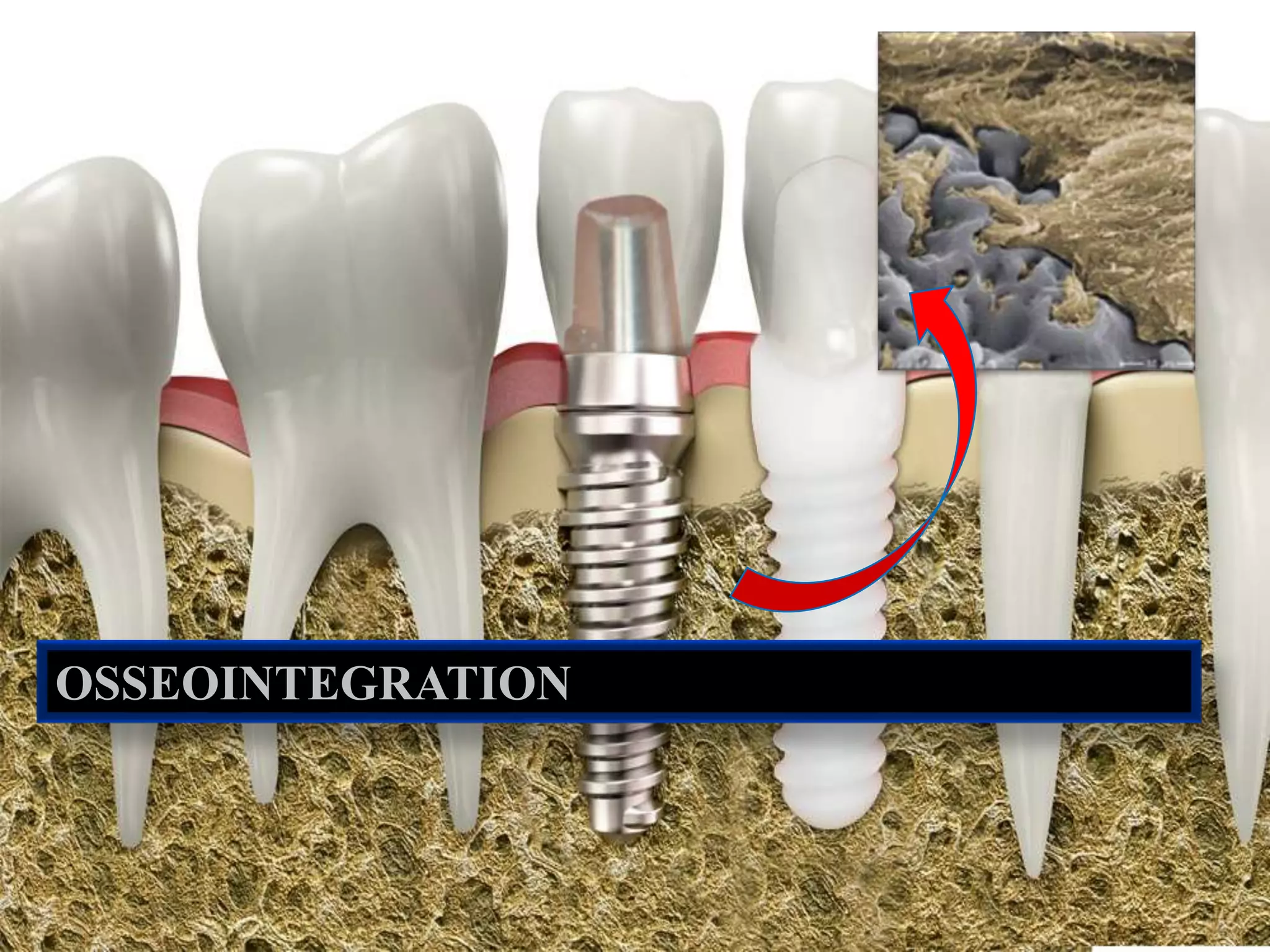
Osseointegration refers to the biological process of direct structural and functional connection between living bone and the surface of dental implants, a concept pioneered by Dr. Per-Ingvar Branemark. The process involves multiple stages of bone healing and integration influenced by various factors related to the patient, surgical methodologies, and implant design. A comprehensive understanding of these variables is critical for successful implementation and long-term efficacy of dental implants.