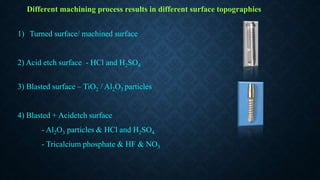
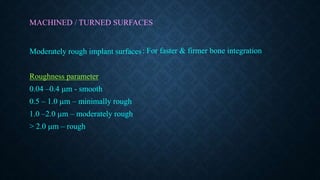
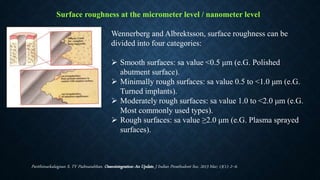
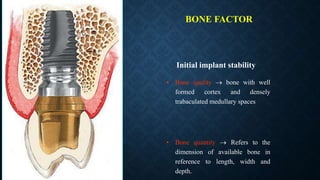
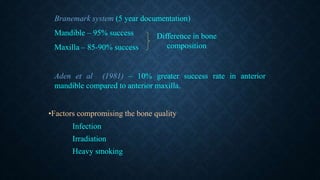
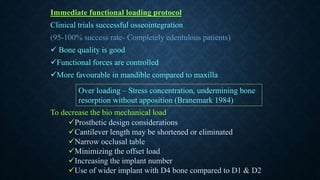
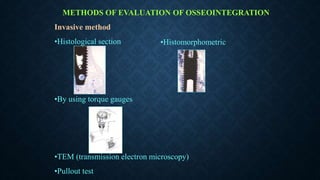
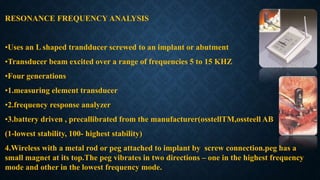
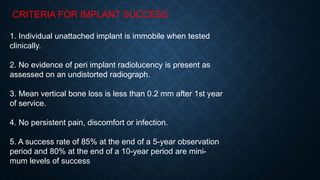
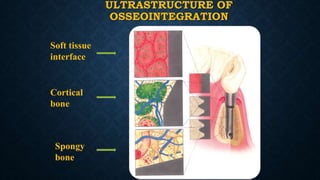
This document discusses osseointegration, the direct attachment of bone to an implant surface without intervening soft tissue. It describes the history and definitions of osseointegration as coined by Dr. Branemark. The mechanism of osseointegration involves inflammation, proliferation, and maturation phases. Factors that enhance osseointegration include implant biocompatibility, design characteristics like surface roughness, and loading conditions. Implant surface characteristics such as texture, energy, and chemistry also impact osseointegration. Moderately rough surfaces generally promote the best bone fixation.





![BONE TO IMPLANT INTERPHASE
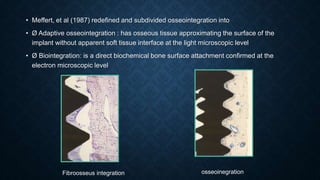
Fibro-osseous integration supported by Linkow (1970),
James (1975), and Weiss (1986) [9],
In 1986, the American Academy of Implant Dentistry defined fibrous integration as “tissue-to-
implant contact with healthy dense collagenous tissue between the implant and bone”
In this theory, col lagen fibers function similarly to Sharpey’s fibers in natural dentition. The fibers
affect bone remodeling where tension is created under optimal loading conditions
(Weiss, 1986).
When the implant is in function the fibers closer to the implant surface gets compressed with a
corresponding tension on the fibers placed or inserting into the trabaculae
It is not accepted now as no sharpey’s fibers are present between the bones and implant so it is
difficult to transmit the loads. Therefore, bone remodeling cannot be expected to occur in fibro-
osseous integration. .](https://image.slidesharecdn.com/osseointegration-200317063502/85/Osseointegration-21-320.jpg)
![Osseointegration supported by Branemark (1985) [5].
• This was first described by strock as early as 1939 and more recently by Branemark et
al [2] in 1952.
• Branemark theorizes that the implant must be protected and completely out of function,
as he envisions a period of healing of at least 1 year, in which new bone is formed close
to the immobile resting implant
• Histologically defined as a direct connection between living bone and load carrying
endosseous implant at the light microscopic level](https://image.slidesharecdn.com/osseointegration-200317063502/85/Osseointegration-22-320.jpg)