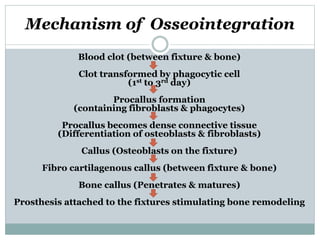
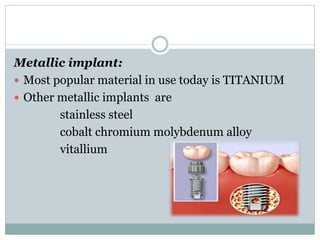
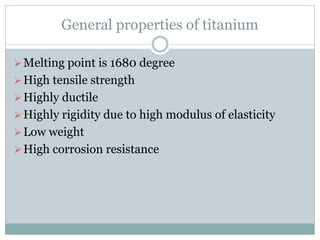
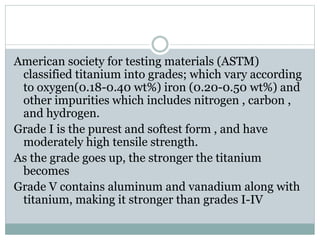
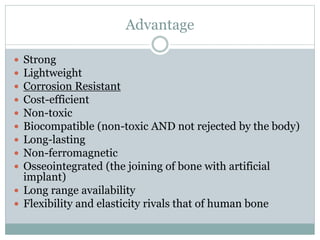
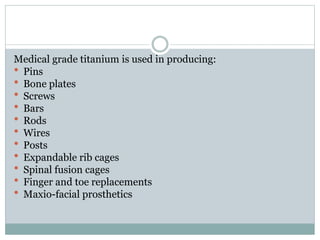
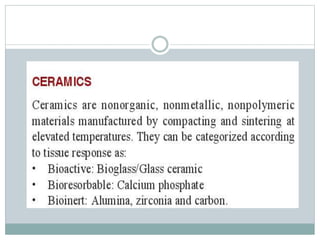
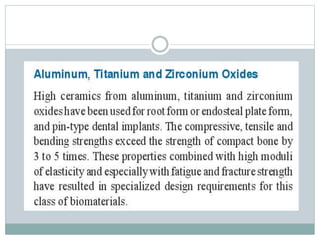
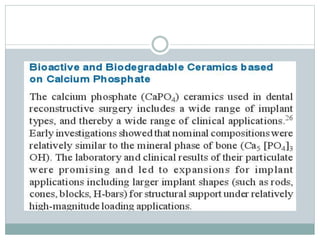
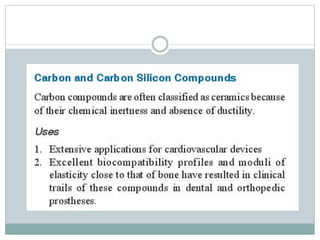
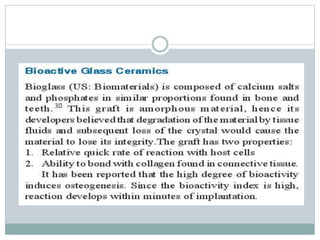
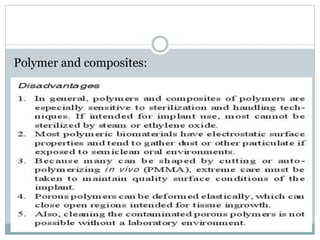
The document discusses implant materials and osseointegration. It describes how implant materials can be classified based on their chemical composition as metals, ceramics, polymers or natural materials. Titanium and its alloys are commonly used metals for implants. Osseointegration is defined as a direct structural and functional connection between bone and the implant surface without intervening soft tissue. The process of osseointegration involves an osteophylic stage of initial bone formation, an osteoconductive stage where bone cells spread along the implant surface, and an osteoadaptive stage of bone thickening in response to loading. Factors like implant design, surface properties and bone quality influence the degree of osseointegr