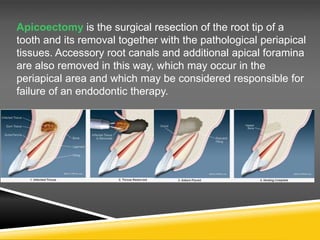
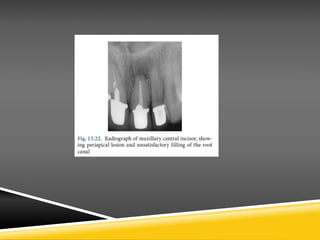
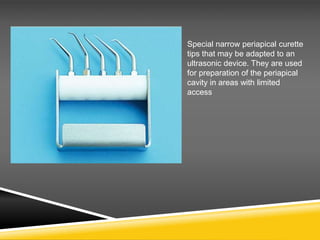
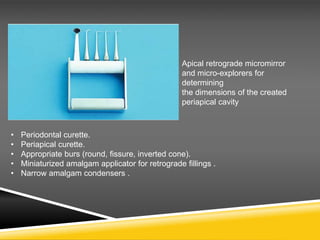
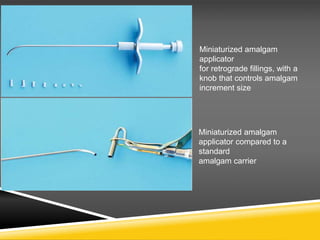
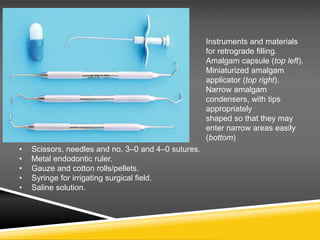
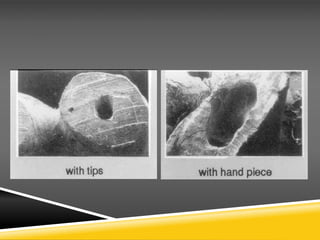
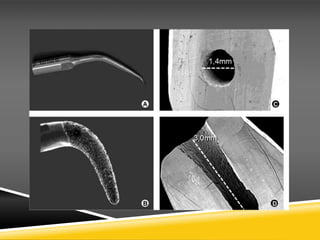
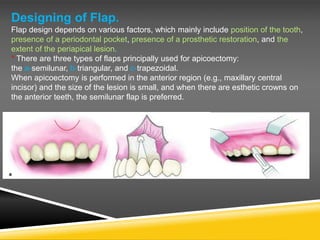
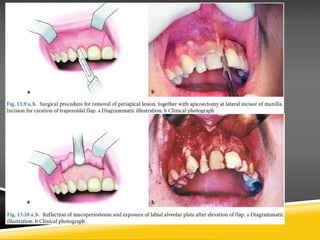
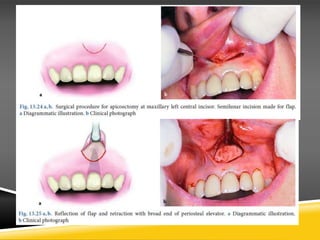
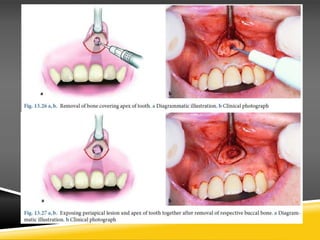
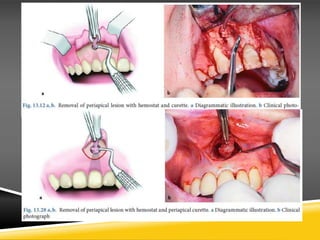
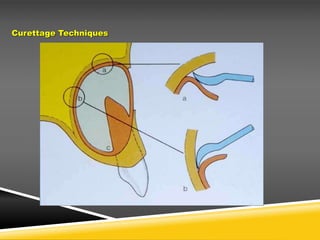
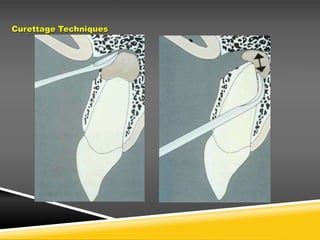
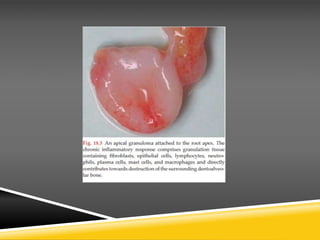
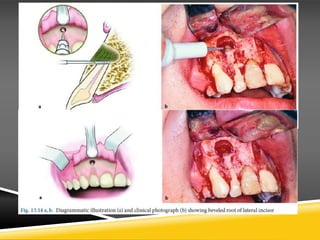
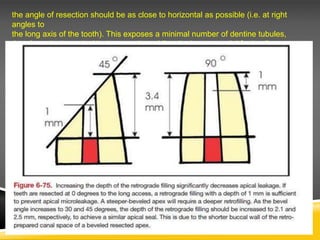
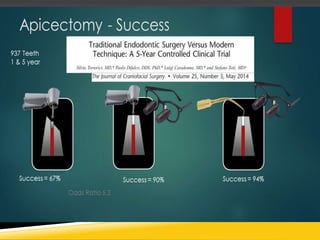
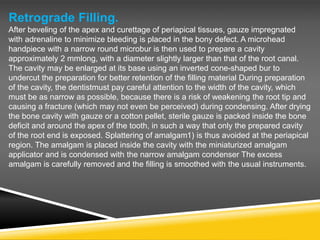
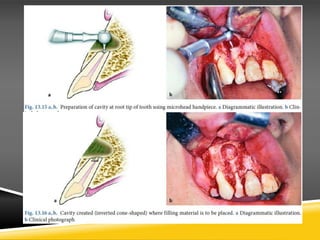
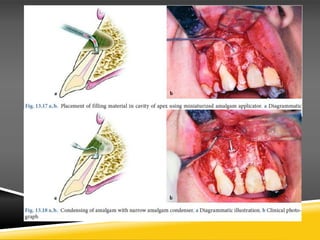
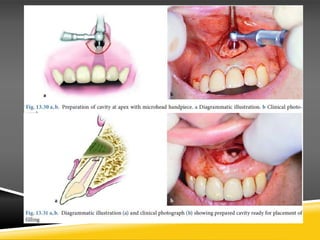
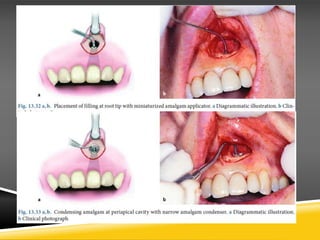
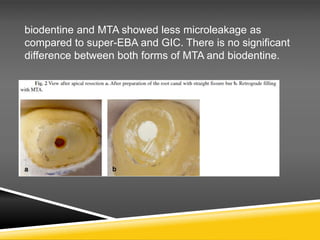
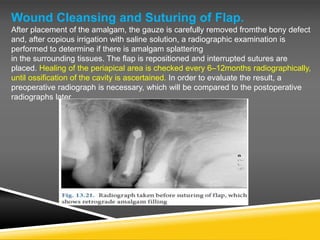
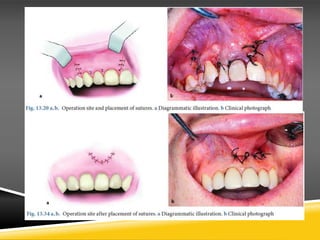
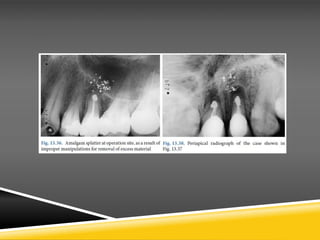
This document provides information on the surgical procedure of apicoectomy. It begins by defining apicoectomy as the surgical resection and removal of the root tip along with pathological tissues. It then lists indications for the procedure such as teeth with active periapical inflammation despite satisfactory endodontic therapy. The document describes the surgical technique which includes flap design, exposing the apex, resection of the apex, and potentially retrograde filling. It provides details on instruments used and cautions to take such as ensuring the resection is at a right angle to reduce apical leakage.