This document appears to be a preface or introduction to a book on orthopaedics written by Dr. J. Maheshwari. It discusses the need for a textbook on orthopaedics that addresses conditions more commonly seen in developing countries. It notes that previous textbooks from Western authors may not adequately cover these conditions. The preface outlines some of the key features of Dr. Maheshwari's book, including starting chapters with relevant anatomy, discussing treatment principles and plans, inclusion of additional chapters on approaches to limb injuries and back pain, emphasis on rehabilitation, and use of diagrams and flowcharts. The goal is to present concepts as clearly as possible for undergraduate medical students and those preparing for postgraduate entrance























![Anatomy of Bone and Fracture Healing | 9
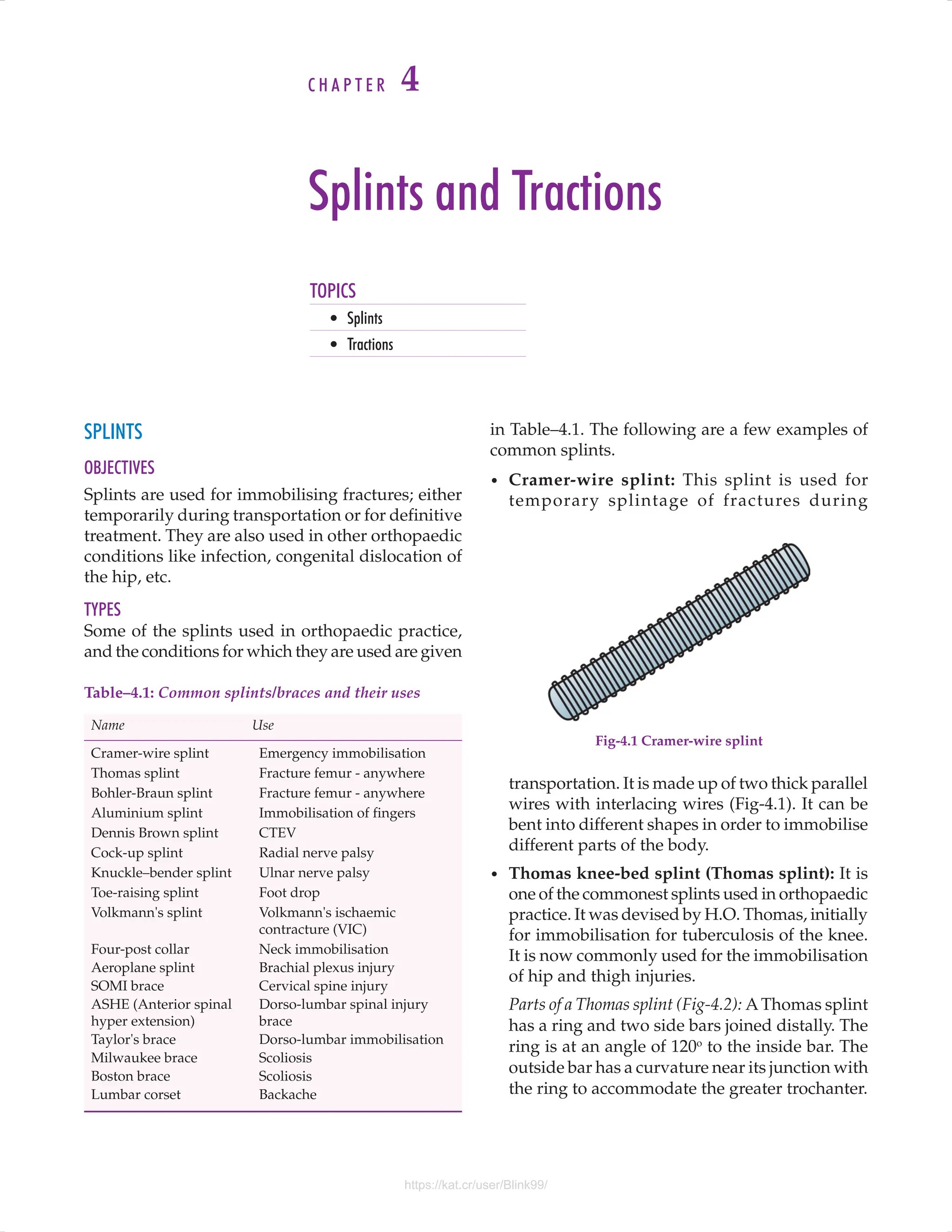
is made up of cortical bone, and the ends mainly
of cancellous bone. The junction between the two,
termed the cortico-cancellous junction is a common
site of fractures (Fig-2.2).
Structural composition of bone: The bone is made
up of bone cells and extra-cellular matrix. The
matrix consists of two types of materials, organic
and inorganic. The organic matrix is formed by the
collagen, which forms 30-35 percent of dry weight
of a bone. The inorganic matrix is primarily calcium
and phosphorus salts, especially hydroxyapatite
[Ca10
(PO4
)6
(OH)2
]. It constitutes about 65-70 percent
of dry weight of a bone.
Bone cells: There are three main cell types in the
bone. These are:
a) Osteoblasts: Concerned with ossification, these
cells are rich in alkaline phosphatase, glycolytic
enzymes and phosphorylases.
b) Osteocytes: These are mature bone cells which
vary in activity, and may assume the form of an
osteoclast or reticulocyte. These cells are rich in
glycogen and PAS positive granules.
c) Osteoclasts: These are multi-nucleate mesen
chymal cells concerned with bone resorption.
These have glycolytic acid hydrolases, collage-
nases and acid phosphatase enzymes.
GROWTH OF A LONG BONE
All long bones, with the exception of the clavicle,
develop from cartilaginous primordia (enchondral
ossification). This type of ossification commences
in the middle of the shaft (primary centre of
ossification) before birth. The secondary ossification
centres (the epiphyses) appear at the ends of the
bone, mostly* after birth.
The bone grows in length by a continuous growth
at the epiphyseal plate. The increase in the girth of
the bone is by subperiosteal new bone deposition.
* The epiphysis of distal end of the femur is present at birth.
At the end of the growth period, the epiphysis
fuses with the diaphysis, and the growth stops. The
secondary centres of ossification, not contributing
to the length of a bone, are termed apophysis (e.g.,
apophysis of the greater trochanter). The time and
sequence of appearance and fusion of epiphysis has
clinical relevance in deciding the true age (bone age)
of a child. Sometimes, an epiphyseal plate may be
wrongly interpreted as a fracture.
Remodelling of bone: Bone has the ability to
alter its size, shape and structure in response to
stress. This happens throughout life though not
perceptible. According to Wolff's law of bone
remodelling, bone hypertrophy occurs in the plane
of stress.
BLOOD SUPPLY OF BONES
There is a standard pattern of the blood supply of a
typical long bone. Blood supply of individual bones
will be discussed wherever considered relevant. The
blood supply of a typical long bone is derived from
the following sources (Fig-2.3):
a) Nutrient artery: This vessel enters the bone
around its middle and divides into two branches,
one running towards either end of the bone.
Fig-2.2 Cortico-cancellous junction
Each of these further divide into a leash of
parallel vessels which run towards the respective
metaphysis.
b) Metaphyseal vessels: These are numerous small
vessels derived from the anastomosis around the
joint. They pierce the metaphysis along the line
of attachment of the joint capsule.
c) Epiphyseal vessels: These are vessels which
enter directly into the epiphysis.
Fig-2.3 Blood supply of a typical long bone
https://kat.cr/user/Blink99/](https://image.slidesharecdn.com/orthopedicsmaheshwari5thedition-231208122354-3db232ed/75/Orthopedics-Maheshwari-5th-edition-pdf-26-2048.jpg)








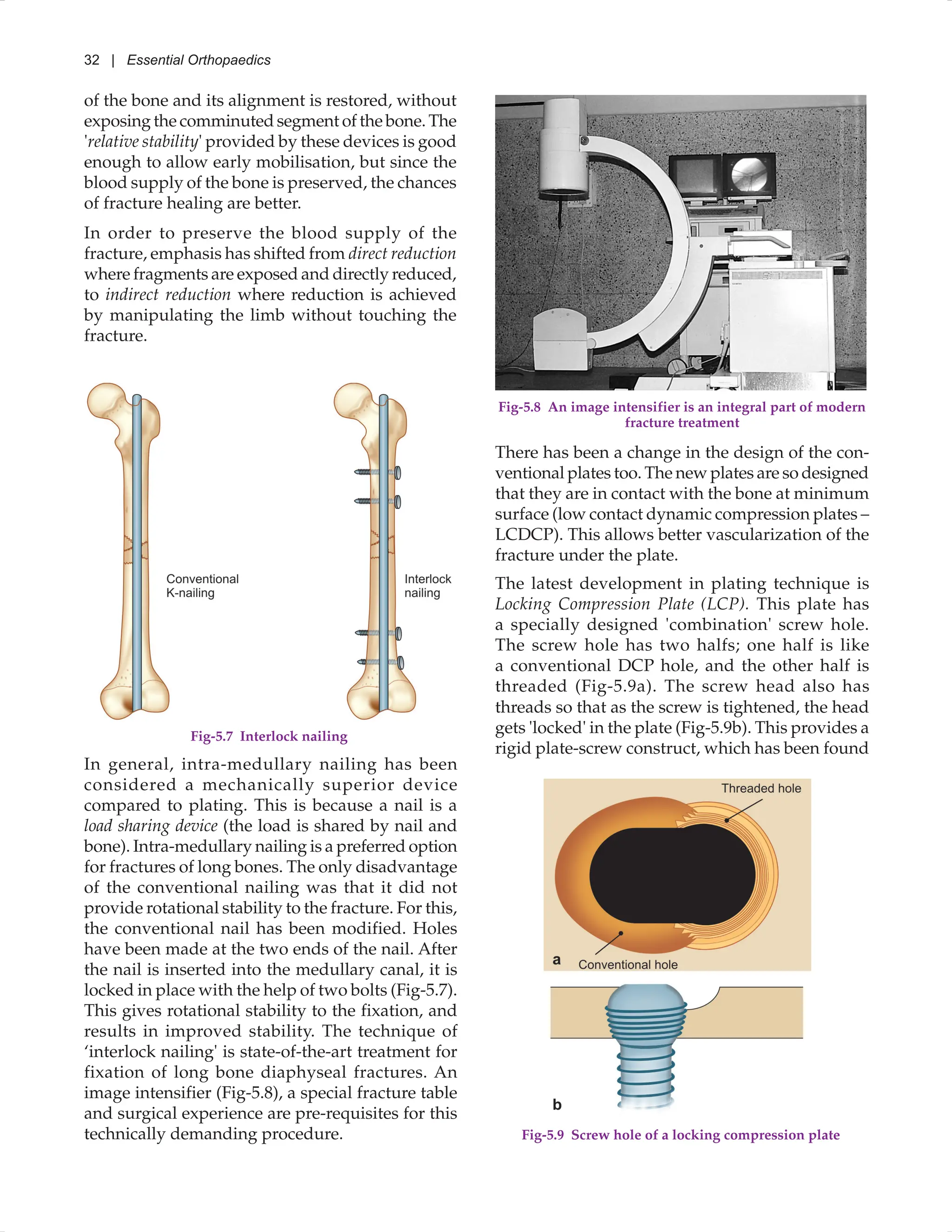
![Treatment of Fractures: General Principles | 19
Advantages of internal fixation: With the use of
modern techniques and implants, there is minimal
need for external immobilisation. It allows early
mobility of the patient out of bed and hospital.
Joints do not get stiff and the muscle functions
remain good. The complications associated with
confinement of a patient to bed are also avoided.
Disadvantages: The disadvantages of internal
fixation are infection and non-union. It needs a
trained orthopaedic surgeon, free availability of
implants and a good operation theatre; failing
which, the results of internal fixation may not only
be poor but disastrous.
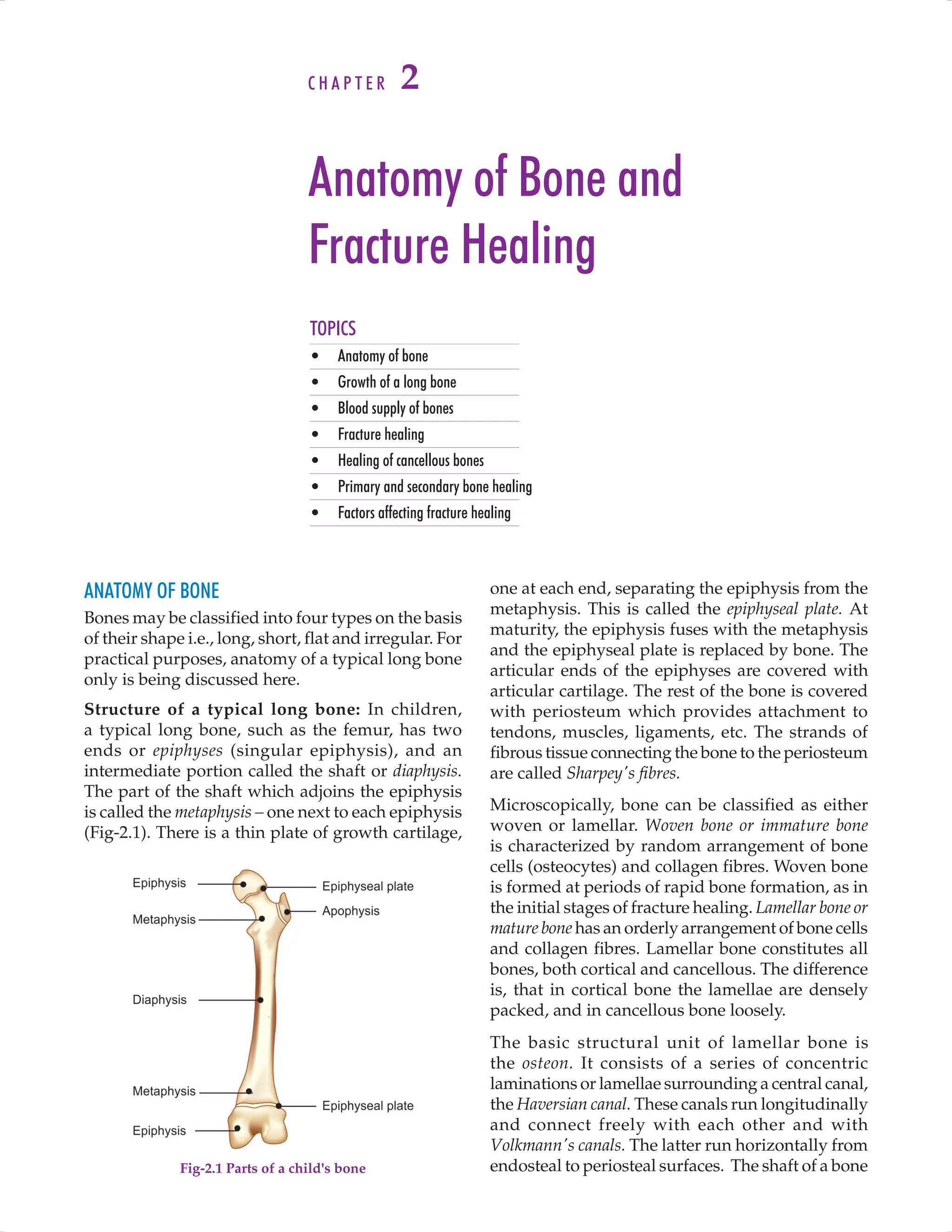
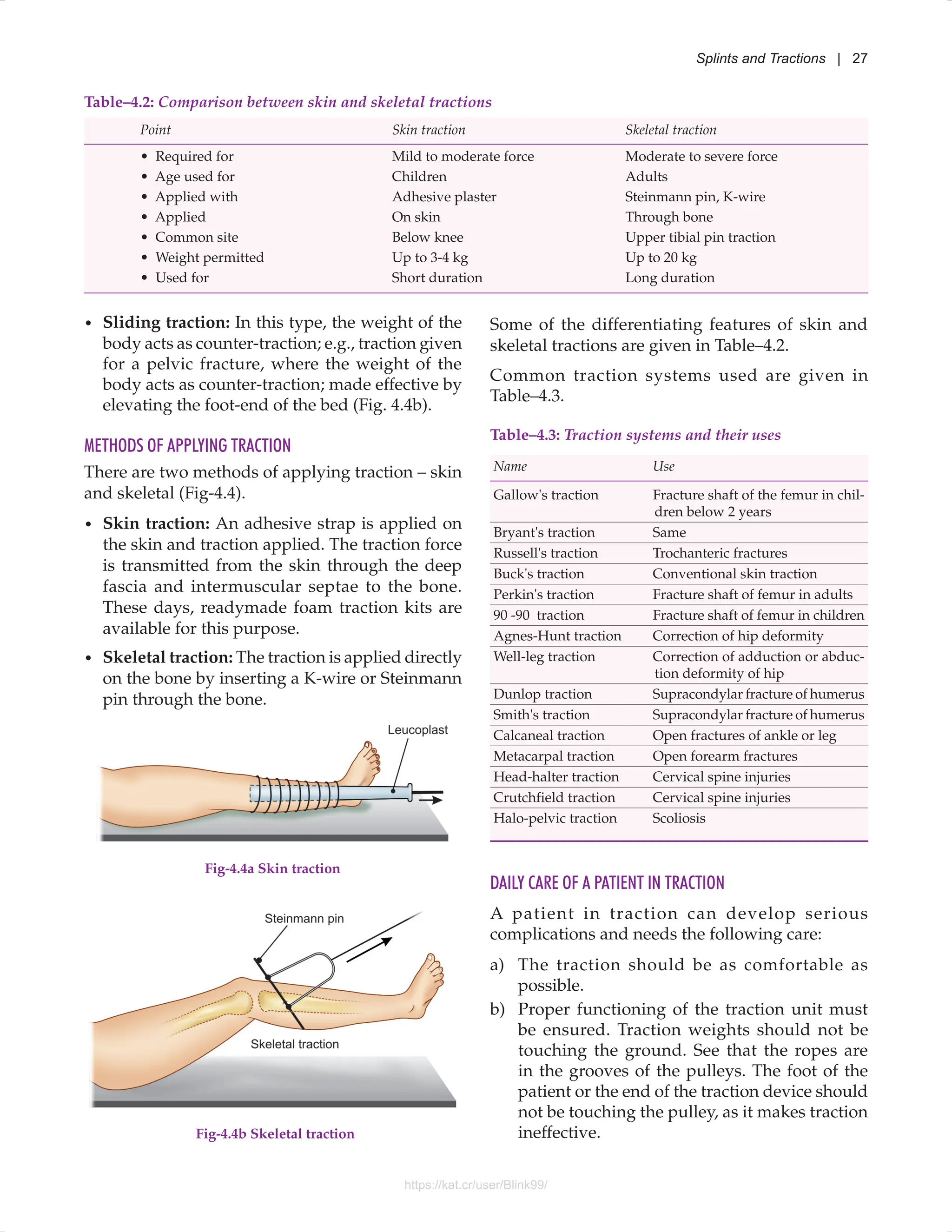
External fixator: It is a device (Fig-3.5) by which the
fracture is held in a steel frame outside the limb.
For this, pins are passed percutaneously to hold
the bone, and are connected outside to a bar with
the help of clamps. This method is useful in the
treatment of open fractures where internal fixation
cannot be carried out due to risk of infection.
These are of the following type:
i. Pin fixators: In these, 3–4 mm sized pins are
passed through the bone. The same are held
outside the bone with the help of a variety of
tubular rods and clamps [Fig-3.5 (a)]
ii. Ring fixators: In thesethin ‘K’ wires (1–2 mm)
are passed through the bone. The same are held
outside the bone with rings [Fig-3.5 (b)], (For
details, page 32).
PHASE III - REHABILITATION OF A FRACTURED LIMB
Rehabilitation of a fractured limb begins at the
time of injury, and goes on till maximum possible
functions have been regained. It consists of joint
Fig-3.5 External fixator. (a) Pin fixator; (b) Ring fixator
Table–3.3 Some implants used in treatment of fractures
Intra-medullary nails
PFN, DFN, PHN, Recon nail supracondylar nail
• Kuntscher's nail Fracture shaft femur
• Smith-Petersen nail Fracture neck femur
• Talwalkar's nail Fracture forearm bones
• V-nail Fracture tibia
• Ender's nail Intertrochanteric fracture
• Rush nail General purpose
• Hartshill rectangle Spine injuries
• GK nail Fracture shaft femur
• Gamma nail Intertrochanteric fracture
Plates and screws
• Compression plate Transverse and oblique
fractures of any long bone
• Neutralisation plate Comminuted fractures
• Buttress plate Condylar fracture of tibia
• Locking compression Peri-articular fractures
plate
Special implants
• SP nail-plate Intertrochanteric fracture
• Dynamic hip screw Intertrochanteric fracture
(DHS)
• Condylar blade-plate Condylar fracture of femur
• T-plate Condylar fracture of tibia
• Spoon plate Fracture of lower end of
tibia
• Cobra plate Hip arthrodesis
Others
• Steel wire Fracture of patella
• K-wire Fracture of small bones
of stainless steel. This can be introduced into
the medullary cavity of the long bones such as
femur and tibia. Different shapes and sizes of
these nails are available.
d) Screws: These can be used for fixing small
fragments of bone to the main bone (e.g., for
fixation of medial malleolus).
e) Plate and screws: This is a device which can
be fixed on the surface of a bone with the help of
screws. Different thicknesses, shapes and sizes
are available.
f) Special, fracture specific implants: These
are used for internal fixation of some fractures
(Table–3.3).
g) Combination: A combination of the above
mentioned implants can be used for a given
fracture.
For details about commonly used implants, refer to
Annexure–I, page 343.
a b
https://kat.cr/user/Blink99/](https://image.slidesharecdn.com/orthopedicsmaheshwari5thedition-231208122354-3db232ed/75/Orthopedics-Maheshwari-5th-edition-pdf-36-2048.jpg)

























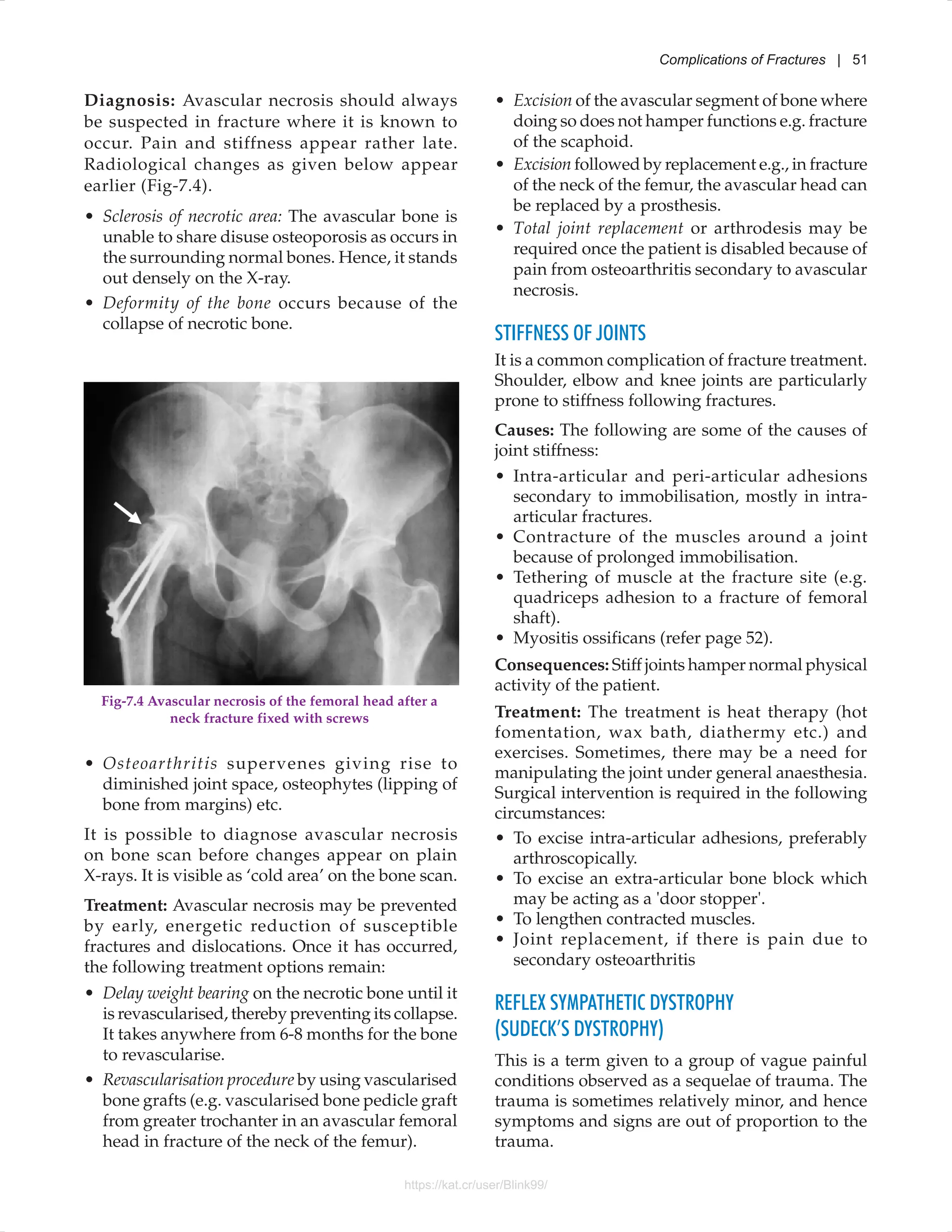
































































![The hand is an important functional unit of
the upper limb without which the whole of the
upper limb becomes almost useless. This calls
for adequate treatment of all hand injuries, how-
so-ever minor they may appear. The following
discussion includes only the important hand
injuries.
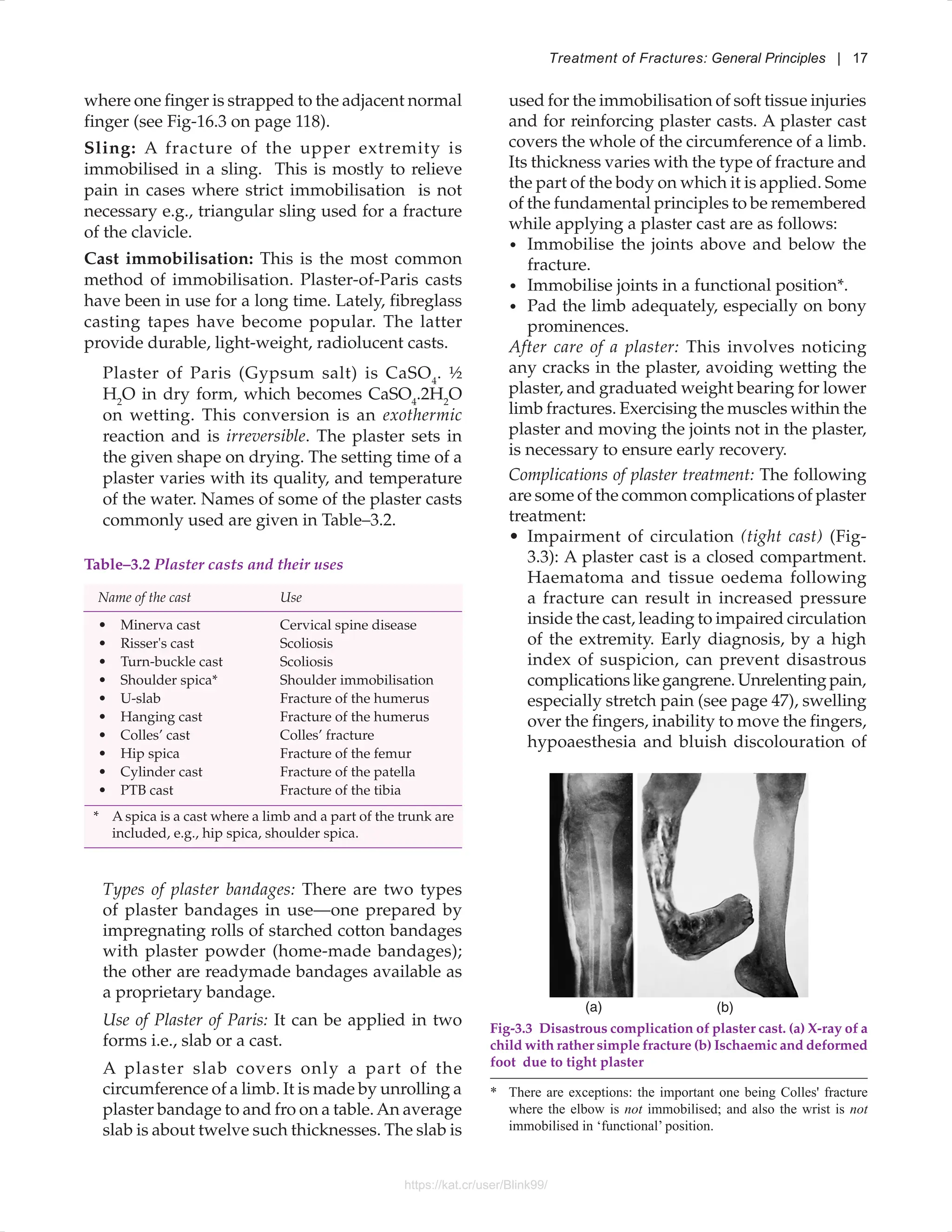
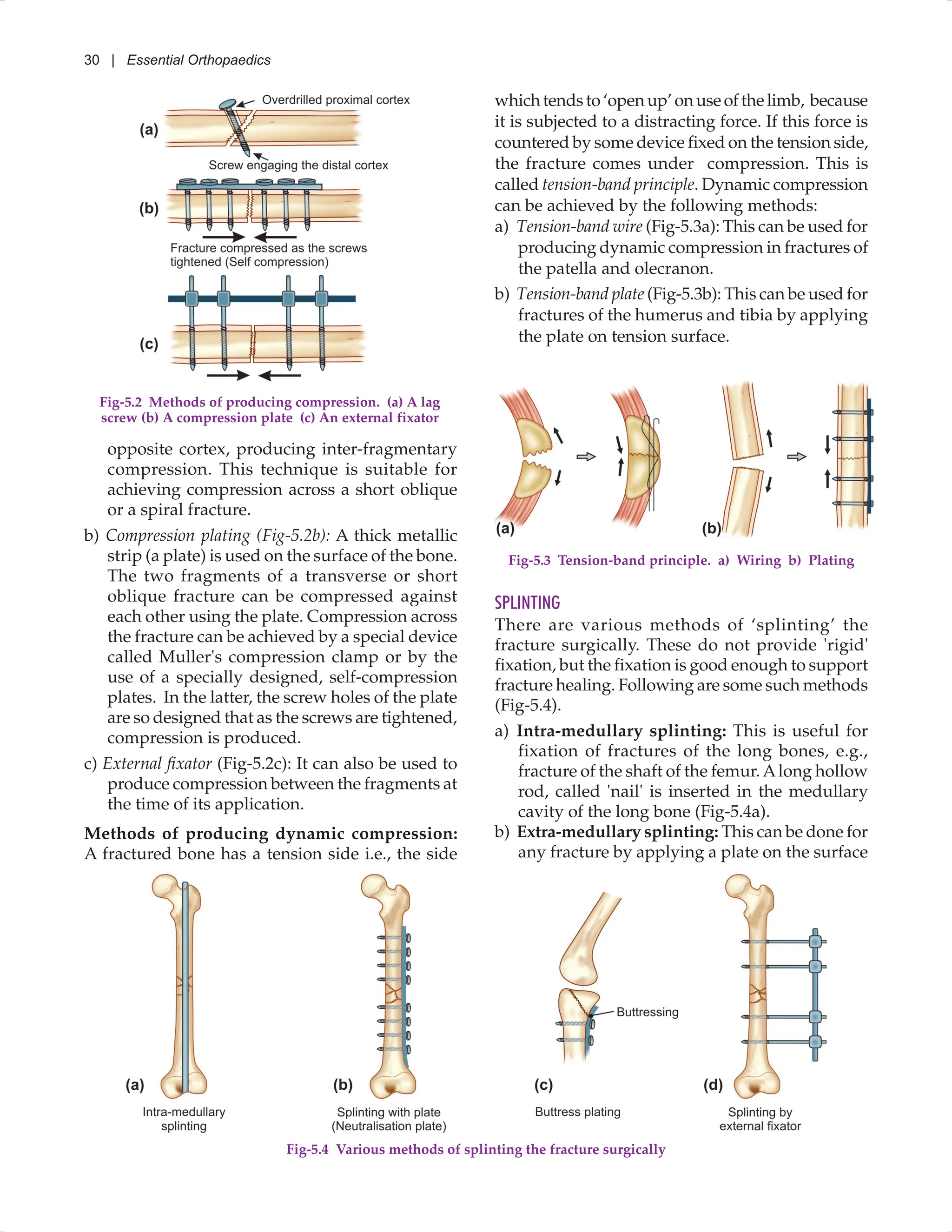
BENNETT'S FRACTURE-DISLOCATION
It is an oblique intra-articular fracture of the
base of the first metacarpal with subluxation
or dislocation of the metacarpal [Fig-16.1(a)]. It
is sustained as a result of a longitudinal force
applied to the thumb.
TREATMENT
Accurate reduction and restoration of the smooth
joint surface is important. This is because, being an
intra-articular fracture, if not reduced accurately,
it will lead to incongruity of the articular surfaces.
Fig-16.2 X-rays showing Bennett's fracture-dislocation
fixed with K-wire
TOPICS
• Bennett's fracture-dislocation • Dislocation of the metacarpo-phalangeal joints
• Rolando's fracture • Amputation of fingers – principles of treatment
• Fractures of the metacarpals • Tendon injuries of the hand
• Fractures of the phalanges • Crush injury to the hand
Hand Injuries
C H A P T E R 16
This would increase the chances of developing
osteoarthritis. The following methods of treatment
are used:
a) Closed reduction and percutaneous K-wire
fixation under an image intensifier, is a good
technique. K-wire is used and incorporated in
a plaster cast (Fig-16.2).
b) Open reduction and internal fixation with a
K-wire or a screw may be necessary in some
cases.
COMPLICATIONS
Osteoarthritis develops if the joint surface is left
irregular. It may cause persistent pain and loss of
grip, so the patient is disabled when attempting
heavy work. Excision of the trapezium may be
required in particularly painful arthritis cases.
Fig-16.1 (a) Bennett's fracture. (b) Rolando's fracture
https://kat.cr/user/Blink99/](https://image.slidesharecdn.com/orthopedicsmaheshwari5thedition-231208122354-3db232ed/75/Orthopedics-Maheshwari-5th-edition-pdf-134-2048.jpg)
![118 | Essential Orthopaedics
TREATMENT
Union is not a problem; the problem is maintaining
proper alignment of the fracture. Treatment is as
follows:
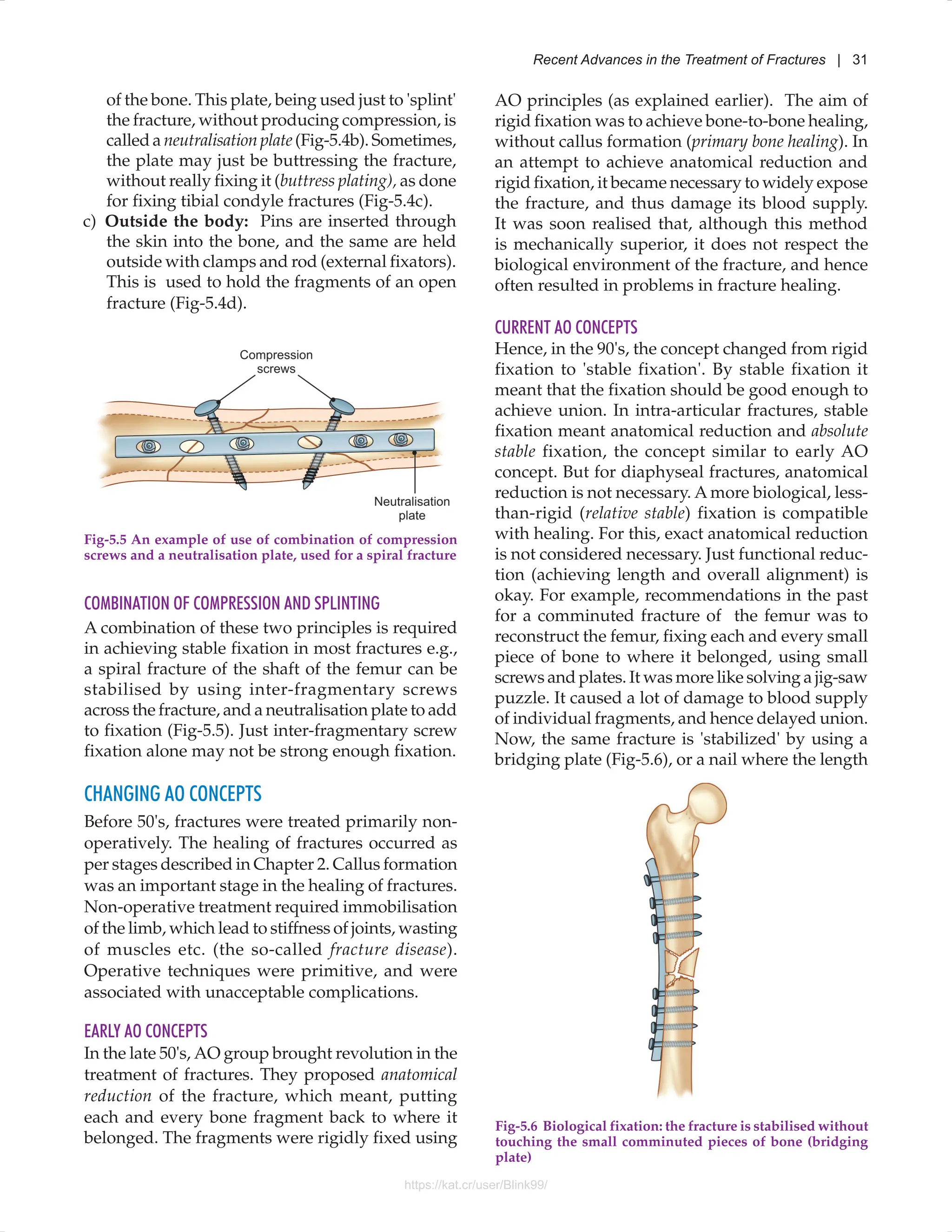
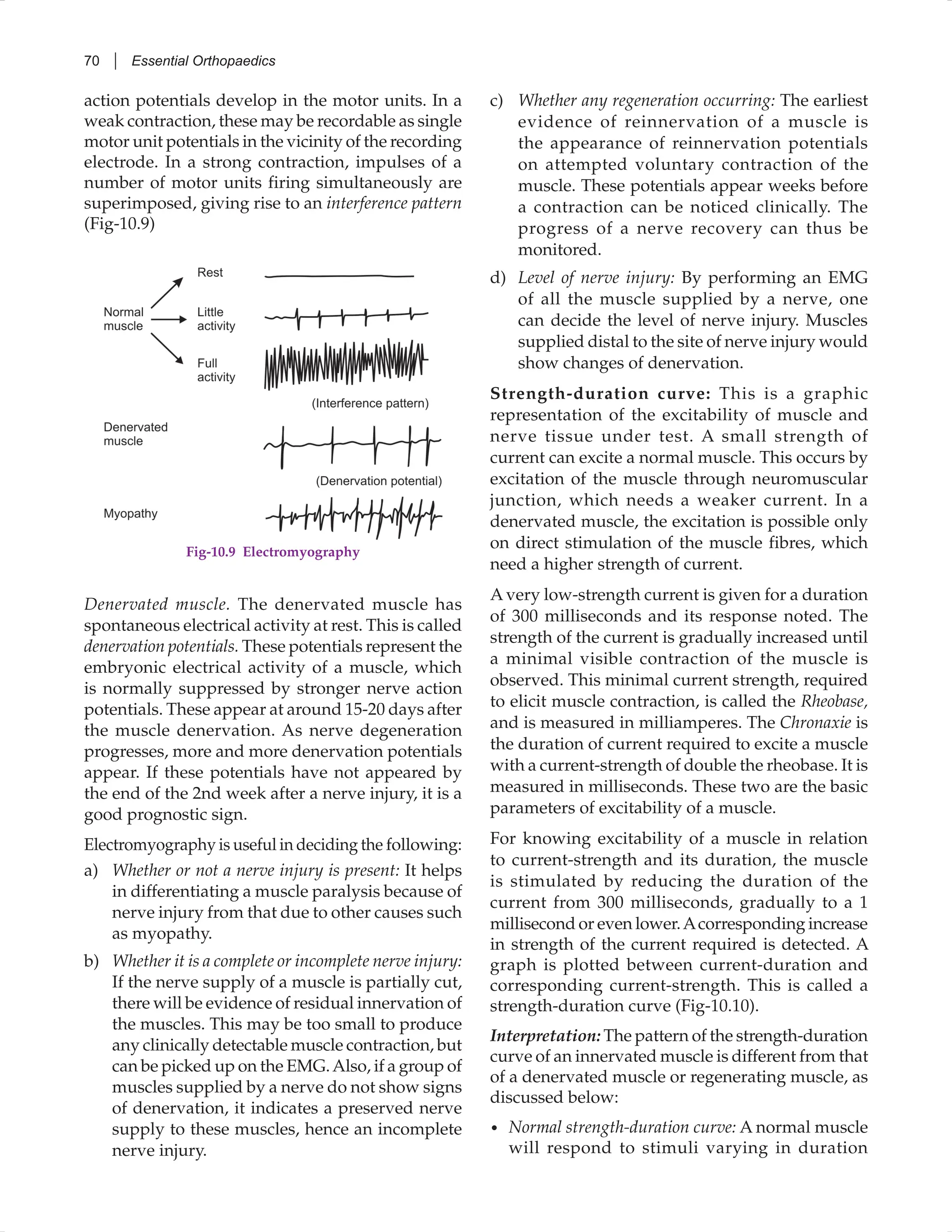
a) Undisplaced fracture: Treatment is basically for
the relief of pain. A simple method of splintage
is to strap the injured finger to an adjacent
finger for 2 weeks (Fig-16.3). After this, finger
mobilisation is started.
ROLANDO'S FRACTURE
This is a complete articular, ‘T’ or ‘Y’ shaped fracture
of the first metacarpal [Fig-16.1(b)] Perfect reduction
is not as important as in Bennett’s fracture-
dislocation. Treatment is by accurate reduction
and fixation with ‘K1
’ wires and immobilisation in
a thumb spica for 3 weeks.
FRACTURES OF THE METACARPALS
Fractures of the metacarpal shaft are common at all
ages. The common causes are: (i) a fall on the hand,
(ii) a blow on the knuckles (as in boxing) and (iii)
crushing of the hand under a heavy object. Fracture
of one or more metacarpals may occur. The fracture
may be classified, according to the site, as follows:
a) Fracture through the base of the metacarpal,
usually transverse and undisplaced.
b) Fracture through the shaft – transverse or
oblique. These fractures are usually not much
displaced because of the splinting effect of the
interossei muscles and adjacent metacarpals.
When more than one metacarpal shafts are
fractured,this “auto-immobilisation”advantage
is lost. Such fractures are unstable and require
operative treatment.
c) Fracture through the neck of the metacarpal
– It commonly affects the neck of the fifth
metacarpal. The distal fragment is tilted
forwards. It is usually sustained when a closed
fist hits against a hard object (Boxer's fracture).
TREATMENT
Conservative treatment is sufficient in most cases.
It consists of immobilisation of the hand in a light
dorsal slab for 3 weeks. A minimal displacement is
acceptable, but in cases with severe displacement or
angulation, reduction is necessary. This is achieved
in most cases by closed reduction; in some, par-
ticularly those with multiple metacarpal fractures,
internal fixation with K-wires or mini plates may
be required.
FRACTURES OF THE PHALANGES
These are common fractures, generally sustained
by fall of a heavy object on the finger or crushing
of fingers. The fractures can have various patterns,
and may be displaced or undisplaced.
Fig-16.3 Finger strapping
b) Displaced fracture: An attempt should be made
to reduce the fracture by manipulation, and
immobilised in a simple malleable aluminium
splint.Active exercises must be started not later
than 3 weeks after the injury. If displacement
cannot be controlled by the above means,
a percutaneous fixation or open reduction
and internal fixation using K-wire, may be
necessary. A comminuted fracture of the tip of
the distal phalanx does not need any special
treatment, and attention should be directed
solely to treatment of any soft tissue injury.
Mallet finger (Baseball finger) results from the
sudden passive flexion of the distal interphalangeal
joint so that the extensor tendon of the distal inter-
phalangeal (DIP) joint is avulsed from its insertion
at the base of the distal phalanx. Sometimes it takes
a fragment of bone with it. Clinically, distal phalanx
is in slight flexion. Treatment is by immobilising
the DIP joint in hyperextension with the help of an
aluminium splint or plaster cast.
DISLOCATION OF THE METACARPO-PHALANGEAL
JOINTS
These are uncommon injuries, resulting from
hyperextension of the metacarpo-phalangeal
(MP) joint, so that the head of the metacarpal](https://image.slidesharecdn.com/orthopedicsmaheshwari5thedition-231208122354-3db232ed/75/Orthopedics-Maheshwari-5th-edition-pdf-135-2048.jpg)








































































































































































































































































