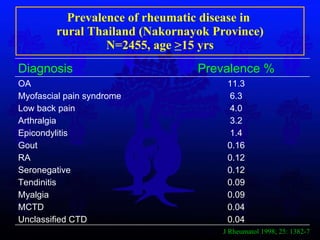
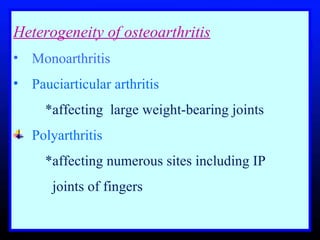
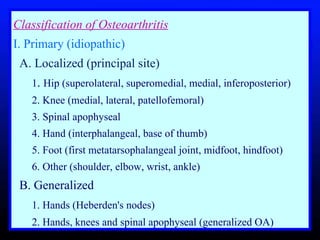
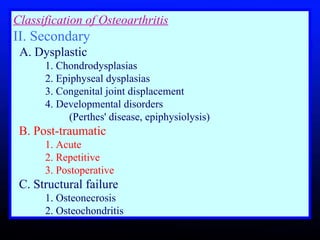
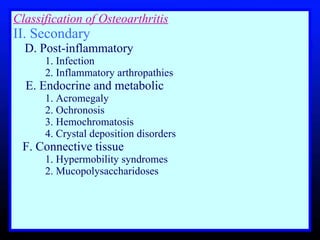
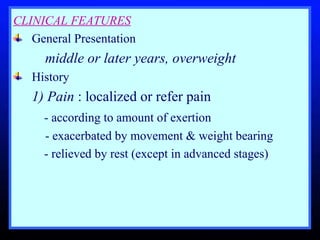
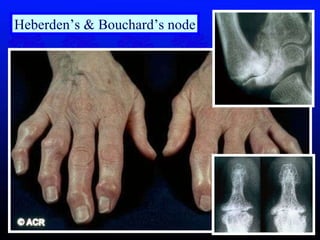
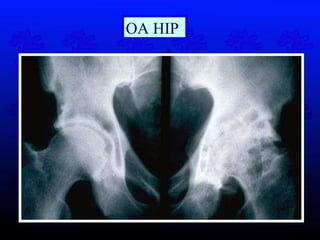
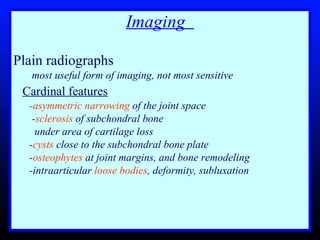
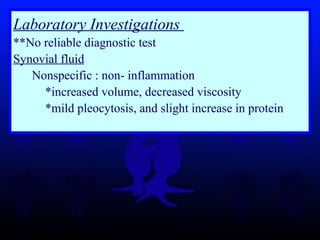
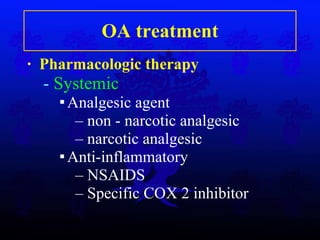
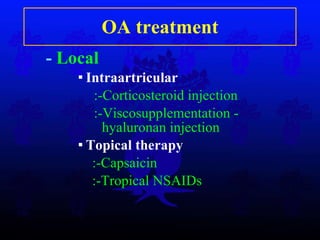
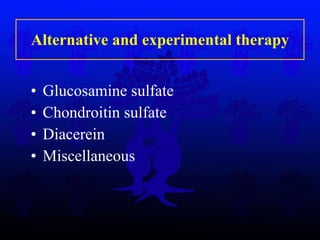
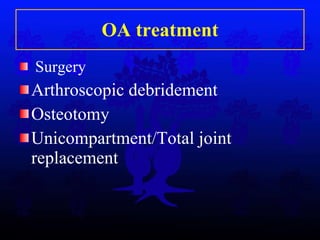
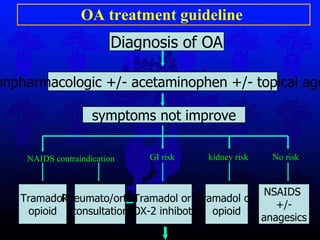
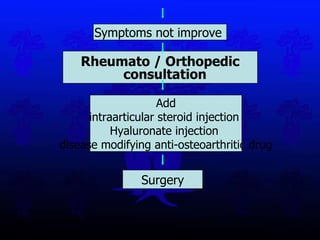
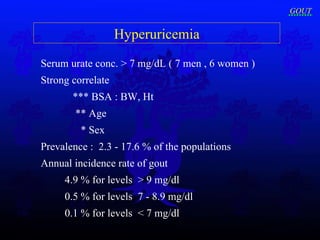
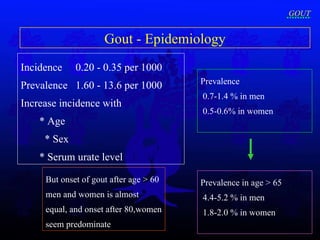
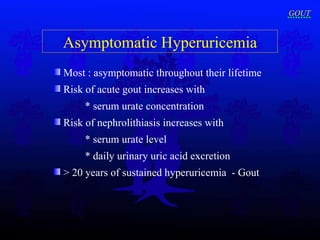
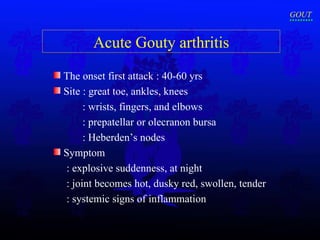
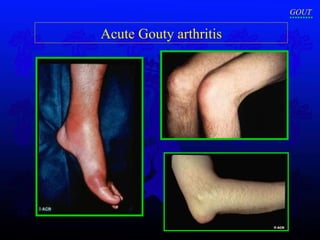
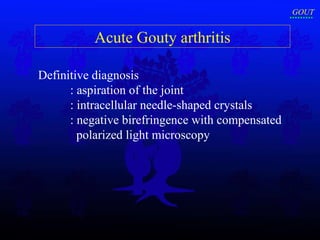
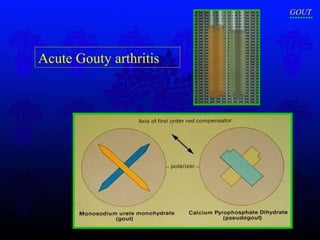
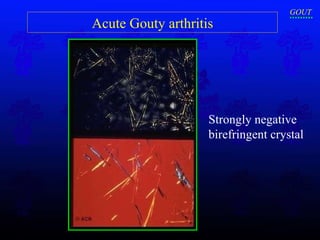
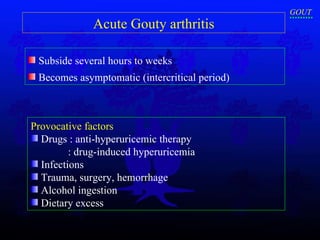
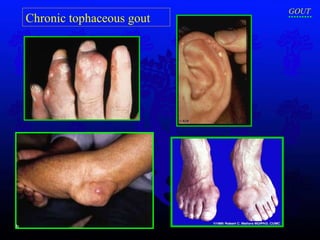
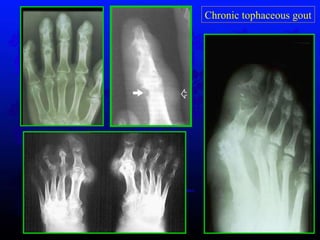
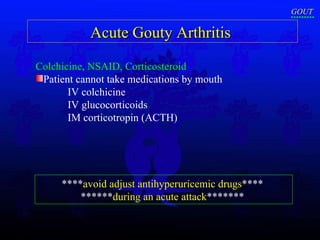
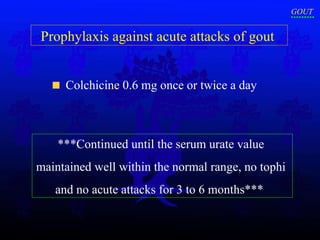
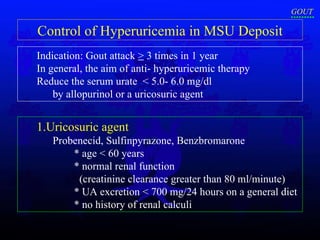
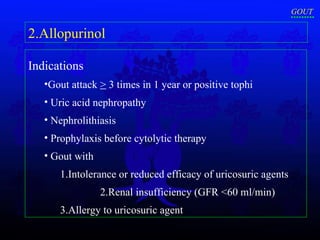
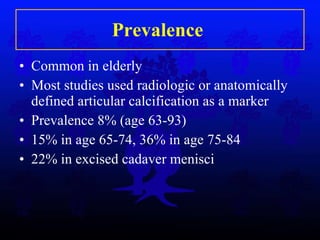
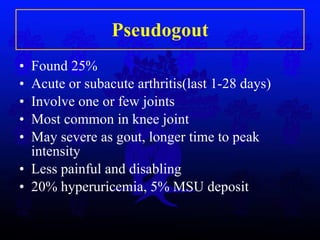
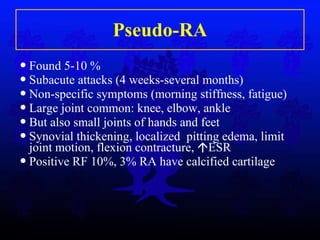
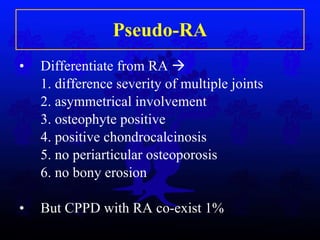
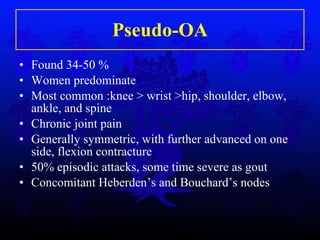
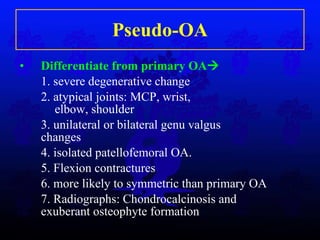
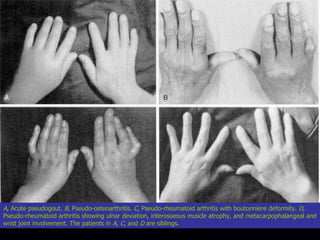
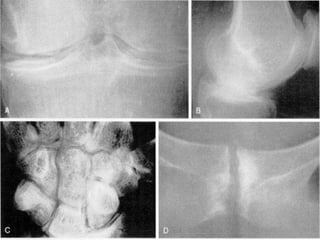
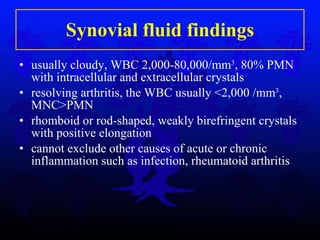
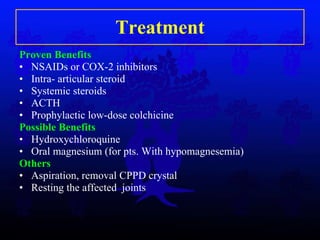
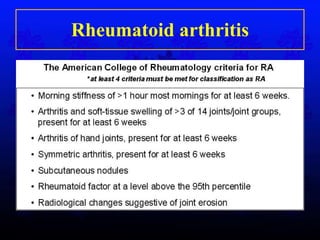
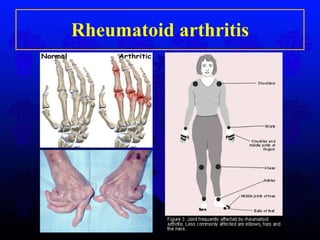
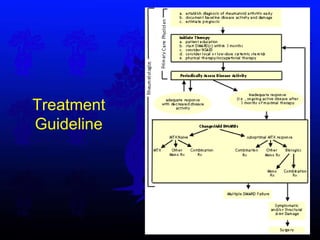
The document discusses several common rheumatological disorders seen in orthopedic departments, including osteoarthritis, gouty arthritis, calcium pyrophosphate deposition disease, and rheumatoid arthritis. It provides details on the prevalence, clinical features, imaging findings, classifications, and treatment approaches for each condition.