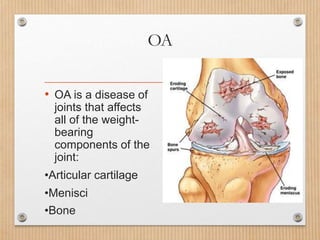
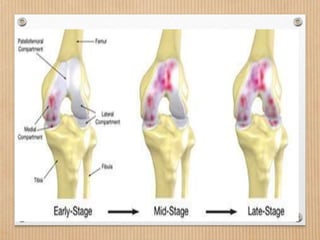
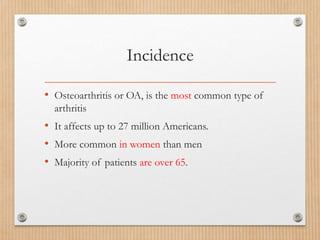
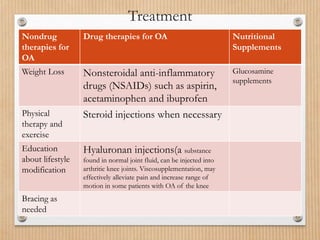
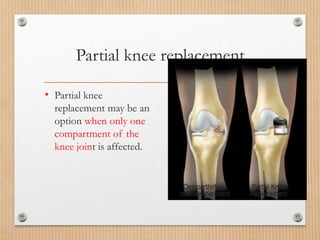
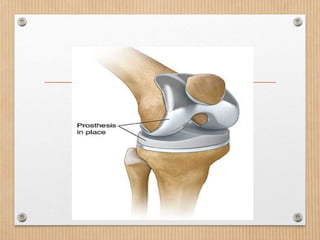
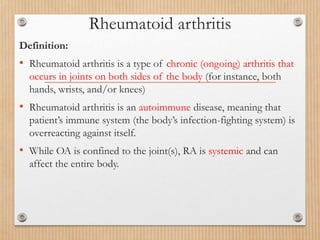
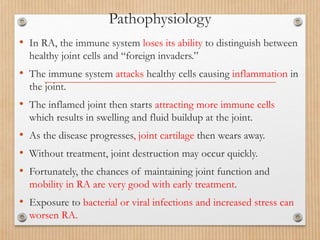
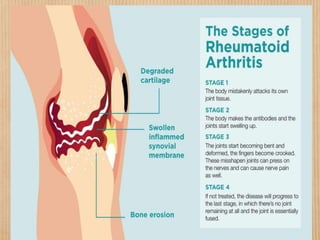
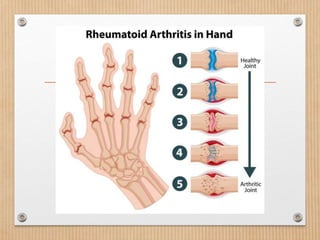
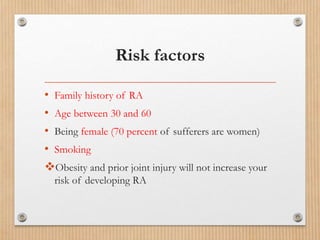
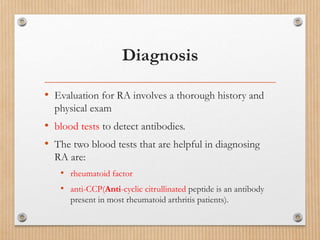
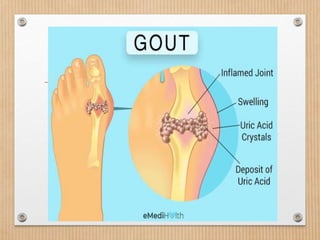
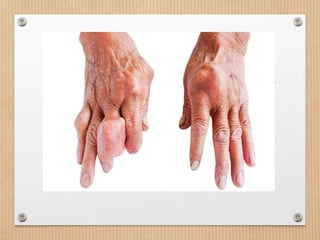
This document provides information on different types of arthritis. It begins by defining arthritis as joint inflammation and pain that limits movement. The three most common types are then described as osteoarthritis, rheumatoid arthritis, and gout. Osteoarthritis is defined as a "wear and tear" type of arthritis that affects cartilage and bone in the joints. Risk factors, symptoms, and treatments are outlined. Rheumatoid arthritis is an autoimmune disease that causes swelling in multiple joints on both sides of the body. Gout involves uric acid crystal buildup in a joint causing sudden severe pain. Diagnosis and management of each type is briefly discussed.