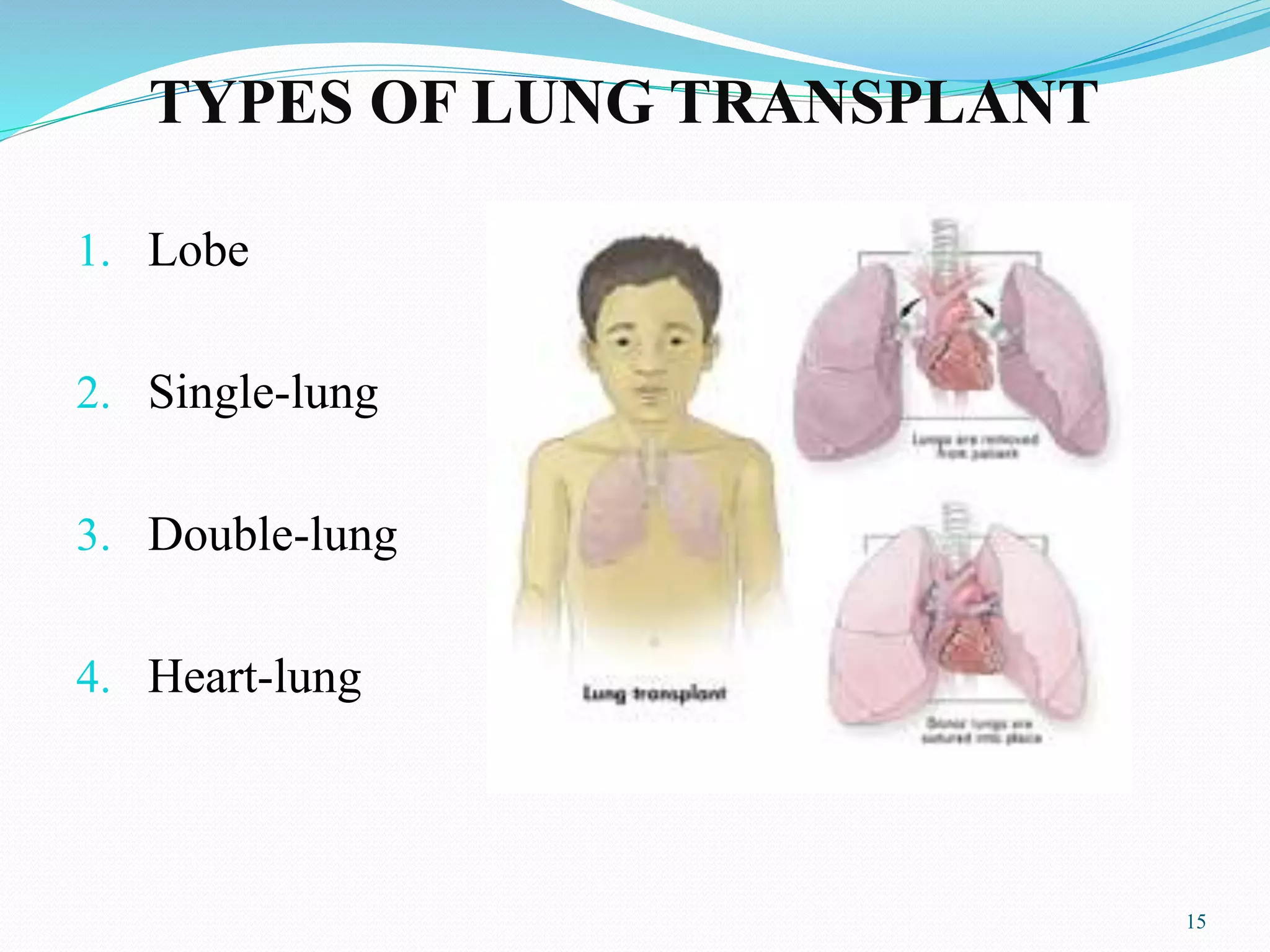
This document provides an overview of organ transplantation. It discusses the history of organ transplantation, including the first successful kidney transplant in 1954. It also outlines the types of organ transplantation, including lung, heart, kidney and more. Requirements for both donors and recipients are explained. Lung transplantation in particular is then discussed in more detail, including qualifying conditions, procedures, post-operative care and risks of infection. The conclusion emphasizes the need for more organ donors to help the thousands of people in need of transplants every year.