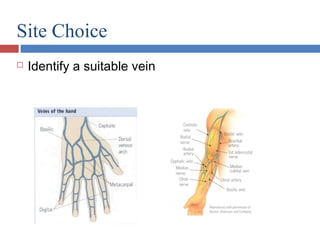
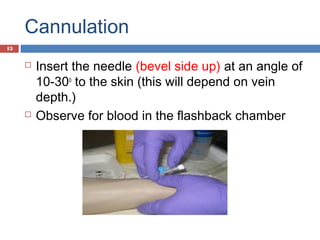
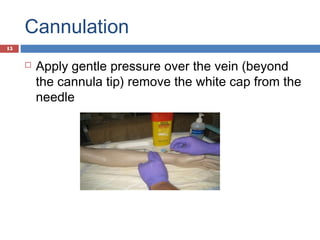
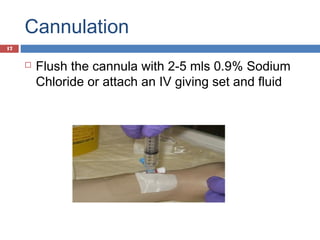
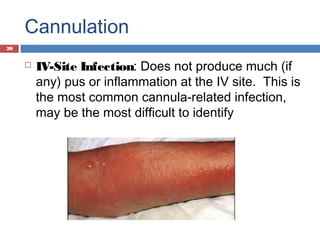
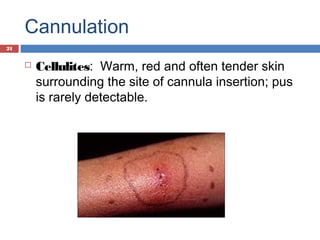
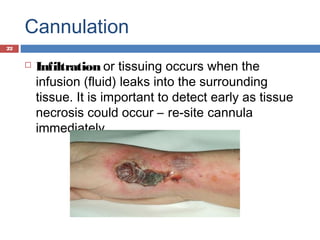
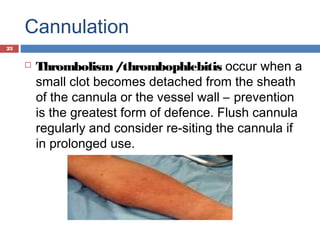
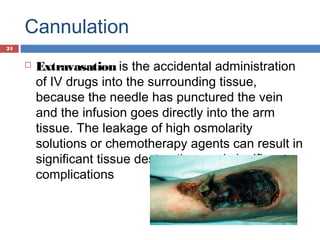
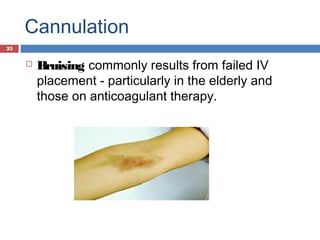
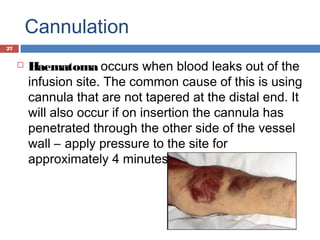
This document provides guidance on intravenous cannulation. It discusses the indications for IV cannulation including fluid replacement, medication administration, blood transfusions, and monitoring. The key steps for cannulation are outlined, including preparing the patient, identifying a suitable vein, inserting the cannula at a 10-30 degree angle, securing the cannula with a dressing, and documenting the procedure. Potential complications from cannulation like infection, infiltration of fluids, thrombosis, and extravasation are also summarized.